Anticholinergic Burden: What It Is and Why It Matters for Medication Safety
When you take more than one medication that blocks acetylcholine, your body builds up what’s called anticholinergic burden, the cumulative effect of drugs that interfere with the neurotransmitter acetylcholine, which controls muscle movement, memory, and other vital functions. Also known as anticholinergic load, it’s not a single drug reaction—it’s the quiet sum of many small hits to your nervous system.
This isn’t just about one pill. It’s about the anticholinergic drugs, medications that reduce acetylcholine activity, commonly used for allergies, overactive bladder, depression, Parkinson’s, and even sleep problems stacking up in your daily routine. Think of common OTC sleep aids, older antidepressants, bladder meds like oxybutynin, or even some stomach drugs. Each one adds a little more pressure on your brain and body. The problem? Many people don’t realize they’re taking any of these—especially if they’re prescribed by different doctors or bought without a prescription. And for older adults, even small amounts can lead to confusion, memory lapses, falls, or worse.
The real danger isn’t always obvious. You might not feel dizzy or foggy right away, but over time, your brain adapts to less acetylcholine—and that’s when things start slipping. Studies show people with high anticholinergic burden are more likely to develop dementia, even years later. It’s not guaranteed, but it’s a risk you can reduce. That’s why checking your full list of meds—prescription, OTC, and herbal—isn’t just smart, it’s necessary. You don’t need to stop everything. You just need to know what’s in your system and whether there are safer alternatives.
Some of the posts here show how common these drugs really are. One talks about how polypharmacy, the use of multiple medications at once, often without clear coordination between providers quietly increases anticholinergic risk. Another explains how switching from a branded bladder med to a generic version might not change the burden at all. There’s even a post about how certain antidepressants and sleep aids can make older patients more prone to falls—exactly because of their anticholinergic properties. These aren’t isolated cases. They’re patterns.
If you’re taking three or more medications, especially if you’re over 65, it’s time to ask: Could any of these be adding to your anticholinergic burden? You don’t have to figure this out alone. Your pharmacist can run a quick check. Your doctor can look for alternatives with less impact on your brain. The goal isn’t to cut everything—it’s to cut the unnecessary, replace the risky, and keep what truly helps.
Below, you’ll find real stories and practical guides from people who’ve faced this exact issue—whether it was switching out a sleep aid, managing bladder meds without the fog, or asking their doctor about hidden drug interactions. These aren’t theoretical warnings. They’re lived experiences. And they show you exactly how to take control before the burden becomes too heavy.
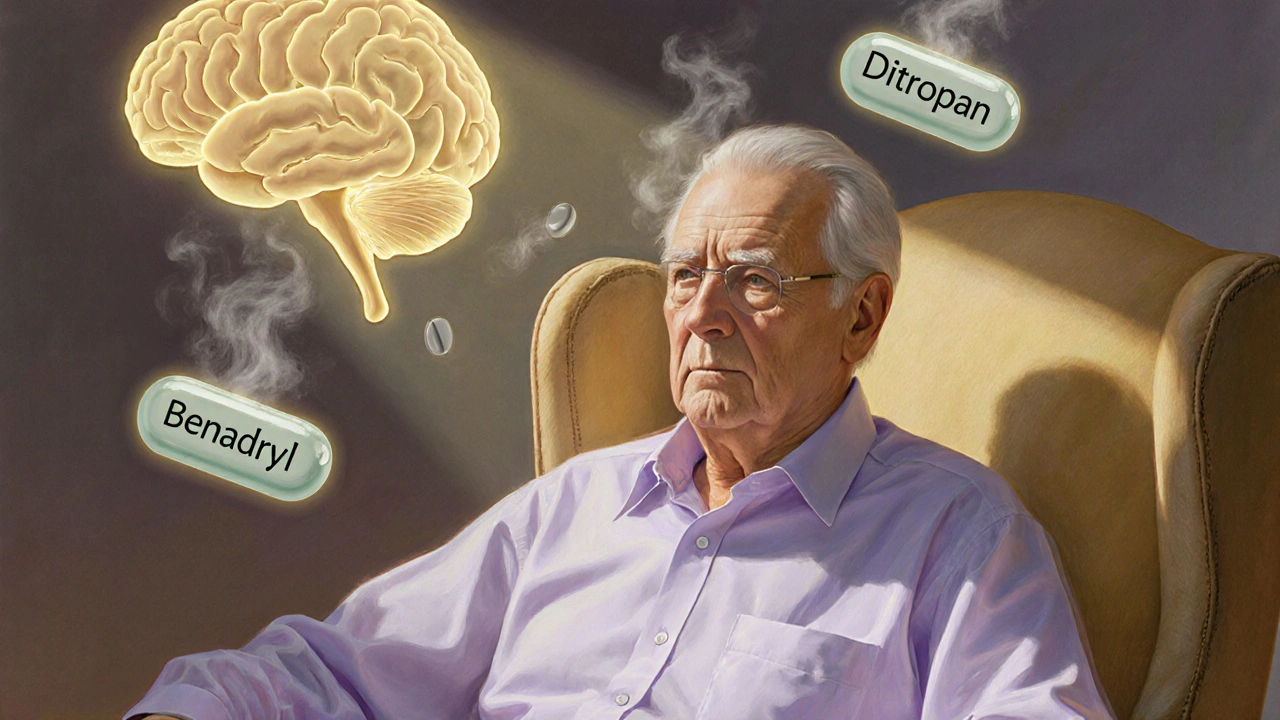
Long-term use of anticholinergic medications like Benadryl, oxybutynin, and amitriptyline is linked to increased dementia risk. Learn which drugs pose the greatest threat, how to check your burden, and safer alternatives.
Read More