Anticholinergic Cognitive Burden Calculator
Medication Assessment Tool
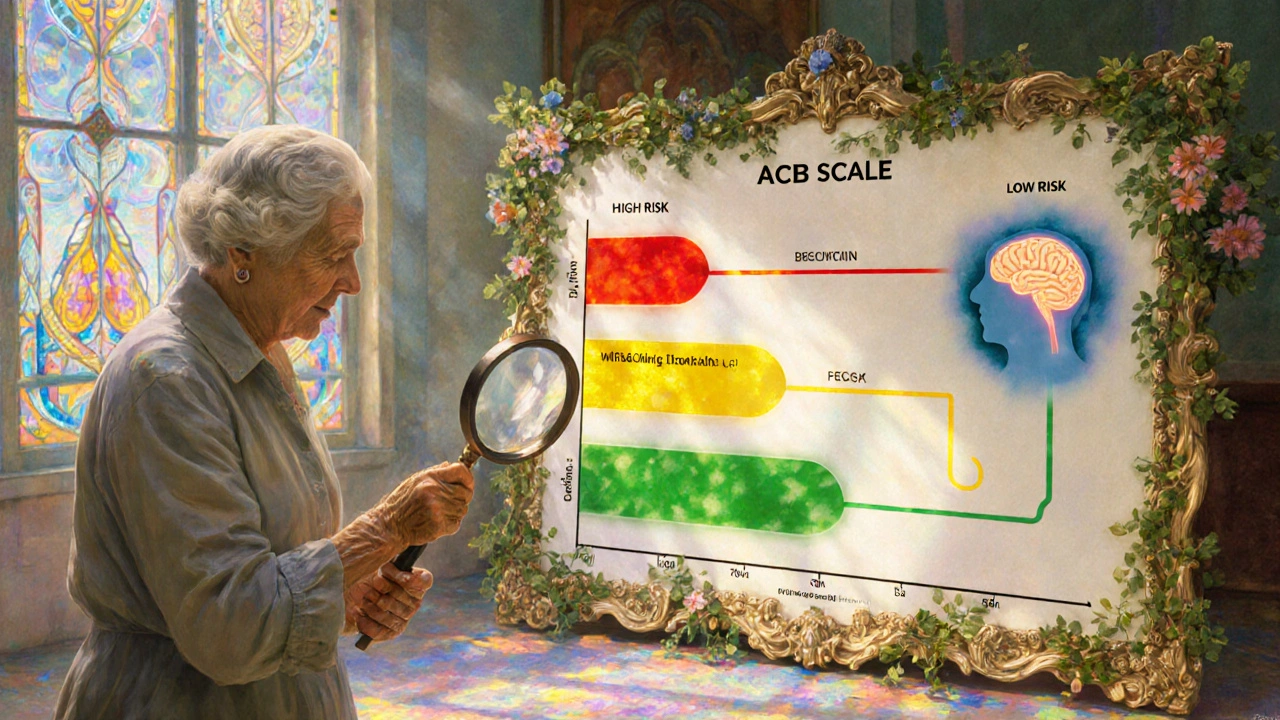
Enter your current medications to calculate your Anticholinergic Cognitive Burden (ACB) score. The ACB scale measures how much each medication affects brain function.
Your Anticholinergic Risk Assessment
Your ACB score indicates your cumulative risk of cognitive decline from these medications.
What your score means
0-1: Low risk - These medications have minimal impact on brain function.
2: Moderate risk - Consider discussing alternatives with your doctor.
3 or higher: High risk - Significant risk of cognitive decline with long-term use. Discuss deprescribing options with your healthcare provider.
Recommended Alternatives
For depression: SSRIs like sertraline or escitalopram are safer alternatives.
For bladder control: Mirabegron (Myrbetriq) has minimal anticholinergic effects.
For allergies: Non-sedating antihistamines like loratadine or cetirizine are better choices.
For insomnia: Cognitive Behavioral Therapy for Insomnia (CBT-I) is more effective long-term.
Many people over 65 take medications for common issues like allergies, overactive bladder, depression, or insomnia. What they might not realize is that some of these everyday pills could be quietly harming their brain. A growing body of research shows that long-term use of anticholinergic medications is linked to a higher risk of dementia and measurable cognitive decline-even in people who seem fine at first.
What Are Anticholinergic Medications?
Anticholinergic drugs work by blocking acetylcholine, a chemical in your brain and body that helps with memory, muscle control, and many automatic functions like digestion and bladder control. These medications have been around for decades and are still widely prescribed. Common ones include diphenhydramine (Benadryl), oxybutynin (Ditropan), amitriptyline (Elavil), and hydroxyzine (Vistaril).
You’ll find them in both prescription and over-the-counter forms. For example, many sleep aids and allergy pills contain diphenhydramine. People take them for everything from hay fever to urinary urgency to chronic pain. But the problem isn’t just taking one pill now and then. It’s the long-term, daily use that adds up.
The Link to Dementia Is Real-And Measurable
Studies tracking tens of thousands of older adults over years have found a clear pattern: the more anticholinergic drugs someone takes, and the longer they take them, the higher their risk of dementia. One major study from the French National Health Insurance database looked at over 1,000 people and found that those who took the equivalent of 1,095 daily doses or more over several years had a 49% higher risk of developing dementia compared to those who didn’t take any.
It’s not just about memory loss. Brain scans show that long-term users have faster shrinkage in areas like the hippocampus-the part of the brain responsible for forming new memories. Glucose metabolism in the brain also drops by 4-8% in these individuals, meaning their brain cells aren’t getting enough energy to function properly.
These aren’t temporary side effects like drowsiness or dry mouth. This is structural, lasting damage. One study found that people on high-anticholinergic drugs lost 0.5-1.2% more brain volume per year than those not taking them. That’s the same rate of decline seen in early Alzheimer’s disease.
Not All Anticholinergics Are Created Equal
Some drugs in this class are far more dangerous than others. The risk isn’t the same across the board. According to research published in JAMA Internal Medicine, antidepressants like amitriptyline carry the highest risk, with a 29% increased chance of dementia. Antipsychotics come next, then bladder medications like oxybutynin and solifenacin.
But here’s something important: trospium, another drug used for overactive bladder, showed no significant link to dementia in the same study. Why? Because it doesn’t cross the blood-brain barrier as easily. That’s a key difference. Drugs that stay mostly outside the brain-like glycopyrrolate or trospium-pose much less risk than those that get inside, like doxepin or amitriptyline.
This means you can’t just say, “All anticholinergics are bad.” You have to look at the specific drug, its strength, and how much of it crosses into the brain. The Anticholinergic Cognitive Burden (ACB) scale helps doctors rate this, with scores of 3 meaning high risk, 2 meaning moderate, and 1 meaning low.
Who’s Most at Risk?
Older adults are the main group affected, but it’s not just age. People who take multiple anticholinergic drugs at once-say, one for sleep, one for bladder control, and one for depression-are at the highest risk. The effects stack up. One pill might not do much. But three or four? That’s when the brain starts to pay the price.
People with a family history of Alzheimer’s or those who carry the APOE-ε4 gene variant are especially vulnerable. That’s why researchers are now running trials like the PREPARE study, which is testing whether stopping these drugs early in high-risk individuals can slow or prevent dementia.
And it’s not just seniors. People in their 50s and 60s who’ve been on these meds for 5-10 years are now showing up with mild cognitive issues. Many don’t connect the dots until it’s too late.
What Patients Are Saying
Real people are seeing the effects. On patient forums, stories like this come up often: “My mom was on amitriptyline for nerve pain for eight years. Her memory got worse. When she stopped it, things didn’t get better-but they didn’t get worse either.”
Others report improvements after switching. One woman switched from oxybutynin to mirabegron for her overactive bladder. Within months, she said she could think more clearly, remember names better, and didn’t feel so foggy in the afternoons.
But here’s the problem: most patients don’t know these drugs can affect their brain. A 2021 survey found that only 37% of primary care doctors routinely check for anticholinergic burden in patients over 65-even though nearly 90% of them agree it’s a risk in theory.
And many patients don’t report cognitive side effects because they assume forgetfulness is just “getting older.” Drugs.com reviews show that only 22% of people taking oxybutynin mention brain fog, even though it’s a known side effect.
What Can You Do?
If you’re on any of these medications, don’t stop cold turkey. Some can cause withdrawal symptoms like increased heart rate, sweating, or even confusion. But you can take action:
- Ask your doctor for a full medication review. Bring in every pill, supplement, and OTC product you take. Ask: “Is this anticholinergic? What’s the ACB score?”
- Look for safer alternatives. For depression, SSRIs like sertraline or escitalopram have little to no anticholinergic effect. For overactive bladder, mirabegron is a good option. For insomnia, cognitive behavioral therapy (CBT-I) works better than sleeping pills long-term.
- Check your OTC meds. Benadryl, Unisom, and many “PM” pain relievers contain diphenhydramine. Switch to non-sedating antihistamines like loratadine or cetirizine.
- Use the ACB scale. You can find free online calculators from the University of Eastern Finland. Plug in your meds and see your total score. A score of 3 or higher is a red flag.
The American Geriatrics Society’s Beers Criteria already lists strong anticholinergics as drugs to avoid in older adults. But awareness is still low. That’s why the Anticholinergic Risk Reduction Initiative aims to cut inappropriate prescribing by 50% by 2027.

What’s Changing in 2025?
Regulators are catching up. The FDA added stronger dementia warnings to 14 anticholinergic drugs in 2020. The European Medicines Agency restricted seven bladder drugs for elderly use in 2021. But patient leaflets still often don’t mention cognitive risks-only 42% of them do, even though EU law requires it.
Meanwhile, drug companies are responding. As of 2023, seven new bladder treatments and three new antidepressants are in late-stage trials-all designed to avoid crossing into the brain. These aren’t just incremental improvements. They’re a shift in design philosophy: treat the condition without hurting the mind.
Experts estimate that reducing anticholinergic exposure could prevent 10-15% of dementia cases each year. That’s over half a million people worldwide who might avoid cognitive decline if we act now.
It’s Not About Fear-It’s About Awareness
No one is saying you can’t take these medications if you need them. Some people rely on them for severe pain, incontinence, or depression that hasn’t responded to anything else. The goal isn’t to scare you. It’s to make sure you know the trade-offs.
If you’ve been on an anticholinergic drug for more than a year, especially if you’re over 60, it’s worth asking: “Is this still the best option?”
Your brain doesn’t always tell you when it’s under stress. But the science is clear: long-term use of these drugs can accelerate cognitive decline. And unlike some other dementia risks-like genetics-you can do something about this one.
Can anticholinergic medications cause dementia?
Yes, long-term use of anticholinergic medications is linked to an increased risk of dementia. Studies show that people who take these drugs for years-especially those with high anticholinergic burden-are more likely to develop cognitive decline and dementia. The risk increases with the total amount taken over time, not just from occasional use.
Which medications have the highest anticholinergic burden?
Tricyclic antidepressants like amitriptyline have the highest risk, followed by antipsychotics and bladder medications like oxybutynin and solifenacin. Over-the-counter sleep aids and allergy pills containing diphenhydramine also rank high. Drugs like trospium and glycopyrrolate have lower brain penetration and carry less risk.
How do I know if I’m taking an anticholinergic drug?
Check the active ingredient on the label. Common ones include diphenhydramine, oxybutynin, amitriptyline, hydroxyzine, and chlorpheniramine. You can also use free online ACB (Anticholinergic Cognitive Burden) calculators or ask your pharmacist to review your list. Many electronic health records now flag these drugs automatically.
Can stopping these drugs improve memory?
In many cases, yes. People who stop high-risk anticholinergics often report clearer thinking, better memory, and less brain fog within weeks to months. While lost brain volume doesn’t fully recover, stopping the drug halts further decline and can stabilize cognitive function. Never stop abruptly-work with your doctor to taper safely.
Are there safe alternatives to anticholinergic drugs?
Yes. For depression, SSRIs like sertraline or escitalopram are preferred. For overactive bladder, mirabegron is a non-anticholinergic option. For insomnia, cognitive behavioral therapy (CBT-I) is more effective long-term than sleeping pills. For allergies, loratadine or cetirizine replace diphenhydramine without the brain effects.
How long does it take for anticholinergic drugs to affect cognition?
Short-term use (less than a year) doesn’t appear to increase dementia risk. But studies show that after 3 or more years of daily use, the risk rises significantly. The damage builds slowly, which is why it’s often missed until cognitive problems become obvious. That’s why early review and deprescribing matter.
Next Steps for Patients and Caregivers
If you’re worried about your meds:
- Make a list of everything you take-prescription, OTC, and supplements.
- Use the ACB scale calculator to get your total burden score.
- Book an appointment with your doctor or pharmacist to review each drug.
- Ask: “Is there a non-anticholinergic alternative?”
- If you’re switching, do it slowly. Withdrawal can cause symptoms if stopped too fast.
Don’t wait until you’re forgetting names or getting lost in familiar places. The brain changes silently. But you don’t have to accept it as normal aging. Knowledge is your best tool-and action, even small steps, can make a real difference.
Neoma Geoghegan
November 23, 2025 AT 19:41ACB score 3? That's a red flag. Time to audit your meds. No more Benadryl sleepers. Swap to loratadine. Your brain will thank you.
Bartholemy Tuite
November 25, 2025 AT 10:15bro i was on amitriptyline for 7 years for back pain and i swear my memory was just... gone. like i'd walk into a room and forget why. stopped it cold turkey because my doc didn't care. woke up 3 months later like i'd been drugged. brain fog lifted. not magic but real. also i switched to gabapentin and miracle i'm still alive. point is: don't assume forgetfulness is aging. it might be your damn allergy pill.
Sam Jepsen
November 26, 2025 AT 03:53Just had this exact convo with my 72-year-old mom last week. She's been on oxybutynin for 10 years and thought her brain fog was just 'getting old.' We pulled up the ACB calculator together - score of 4. She cried. Then we scheduled a med review. She's switching to mirabegron next month. I'm telling everyone. This is the silent epidemic no one talks about.
Yvonne Franklin
November 27, 2025 AT 04:06Check your OTC meds. Unisom, Tylenol PM, Benadryl - all diphenhydramine. Same stuff in 80% of sleep aids. Switch to non-drowsy. Simple. Life-changing. No doctor needed.
Jessica Correa
November 27, 2025 AT 20:08I never realized how many meds I was on that could be doing this. My dad's on three of these and I just thought he was getting forgetful. This makes so much sense now. I'm printing out the ACB scale and taking it to his next appointment
manish chaturvedi
November 28, 2025 AT 03:46In India, these medications are often prescribed without any counseling regarding cognitive risks. Elderly patients are rarely informed that their memory issues may be medication-induced. There is an urgent need for physician education and public awareness campaigns. This is not merely a Western issue.
Nikhil Chaurasia
November 29, 2025 AT 00:10I used to take amitriptyline for migraines. My wife said I was turning into a zombie. I thought she was exaggerating. Then I stopped. Six weeks later, I remembered my daughter's birthday. I cried. I didn't even know I'd forgotten it. These drugs steal pieces of you. Don't wait until you lose the whole picture.
Holly Schumacher
November 29, 2025 AT 05:53Of course the FDA added warnings in 2020. But the real story? The pharmaceutical companies knew this for decades. They just didn't care because they made billions. Your grandma's dementia? Maybe it was their profit margin. Wake up. This isn't science. It's corporate negligence dressed up as medicine.
Michael Fitzpatrick
November 30, 2025 AT 09:35I'm 58 and took diphenhydramine for sleep for 12 years. I thought I was just tired. Turns out I was chemically sedating my brain every night. Switched to CBT-I last year. No pills. Better sleep. Clearer thinking. I feel like I got my brain back. It's not too late. Even if you've been on these for years, stopping can still help. Don't give up.
Shawn Daughhetee
November 30, 2025 AT 10:11my mom took oxybutynin for 8 years and her memory tanked. doc said it was just aging. i found this article and made her stop. she didn't get better but she stopped getting worse. that's a win. also she switched to mirabegron and now she remembers where she put her glasses. small things but they matter
Justin Daniel
December 1, 2025 AT 22:58so you're telling me my grandpa's 'senior moments' were actually just his nightly Benadryl? that's wild. i thought he was just old. turns out he was just drugged. guess we're auditing his medicine cabinet this weekend. thanks for the nudge.
New Yorkers
December 3, 2025 AT 18:32Let me guess - you're the kind of person who thinks dementia is 'preventable' if you just drink kale smoothies and read Kant. Newsflash: your brain isn't a smartphone you can reboot. Some of us need these meds to function. Don't shame people for surviving. Awareness is good. Guilt? Not helpful.