The U.S. Food and Drug Administration (FDA) hasn’t just tweaked its generic drug rules - it’s rewired the entire system. Between 2023 and 2025, the agency rolled out the most significant changes to generic drug approvals since 2012. These aren’t minor updates. They’re a direct response to the broken supply chains that left hospitals scrambling during the pandemic, and they’re reshaping who makes your pills - and how fast you get them.
Why the FDA Changed the Rules
For years, the U.S. relied on foreign factories to make the active ingredients in generic drugs. Over half of all generic medicines sold in America were produced overseas, mostly in India and China. When global shipping slowed or factories shut down, shortages hit hard. Drugs like Ivermectin, Nimodipine, and even basic antibiotics vanished from shelves. The FDA couldn’t inspect foreign plants quickly enough - each trip took 47% longer and cost 32% more than checking a U.S. facility. In 2023, Congress passed the National Defense Authorization Act, demanding the government fix this. The result? Executive Order 14080, which told the FDA: make generic drugs in America. That’s not just a slogan - it’s now a requirement for faster approval.The ANDA Prioritization Pilot Program
On October 3, 2025, the FDA launched the ANDA Prioritization Pilot Program. This isn’t a suggestion. It’s a fast track. If your generic drug is made, tested, and packaged entirely in the U.S., your application gets moved to the front of the line. Here’s how it works:- Tier 1: 100% U.S. manufacturing and testing → target review time: 8 months (down from 12-15)
- Tier 2: 75-99% U.S. components → 10-month review
- Tier 3: 50-74% U.S. components → 12-month review
- Tier 4: Less than 50% U.S. → standard timeline
What’s Getting Approved Faster
The results are already visible. Through mid-2025, the FDA approved nine first generic drugs under this new system. Among them:- Ivermectin Tablet (Application #215922)
- Nimodipine Solution (Application #213409)
- Azilsartan Medoxomil and Chlorthalidone Tablet (Application #217490)
Who Benefits - and Who Struggles
The pilot program gives a huge advantage to manufacturers with U.S. facilities. Companies that use American-made active ingredients and run bioequivalence tests in FDA-registered labs see:- 28% faster time-to-market (11.2 months vs. 15.6 months)
- 41% fewer major deficiency letters
- 33% higher first-cycle approval rates
What’s Not Covered - Yet
The pilot doesn’t include all generics. Complex drugs like transdermal patches, nasal sprays, and ophthalmic suspensions were left out at first. Why? Testing them in the U.S. is harder. Their absorption rates vary wildly based on tiny changes in formulation. But that’s changing. Starting January 2026, the FDA will expand the pilot to include these complex generics. New guidance for nasal sprays and patches is due by November 2025. This could be a turning point - these drugs are often used by elderly and chronically ill patients. If they’re in short supply, people die.The Hidden Costs
The FDA says this program will save $4.2 billion a year by 2030 through fewer emergency drug purchases and hospital shortages. But upfront? It’s expensive. MedPAC, the Medicare advisory group, estimates generic drug prices could rise 12-18% in the next few years as manufacturers pass on facility costs. That’s not just a business problem - it’s a patient problem. Millions rely on generics to afford their prescriptions. The good news? The Congressional Budget Office predicts prices will normalize after 3-5 years as domestic capacity grows. And the FDA’s own data shows 94.7% of pilot participants are happy with the process. They just wish the paperwork wasn’t so heavy.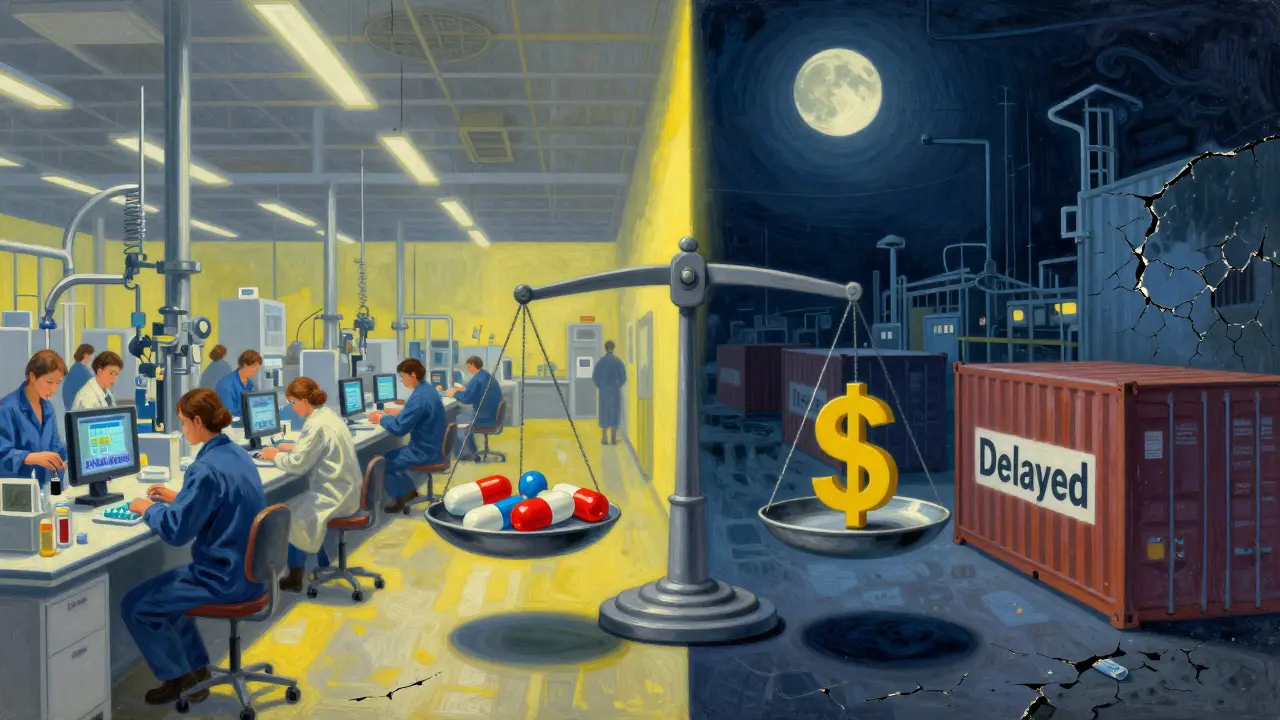
What Manufacturers Must Do Now
If you’re a generic drug maker, here’s what you need to fix right now:- Verify your API source. Is it from a U.S. facility? If not, can you prove it’s equivalent to U.S. standards?
- Move your bioequivalence testing. It must happen in an FDA-registered U.S. lab. Foreign labs don’t count.
- Update your documentation. The FDA requires proof of CGMP compliance for every U.S. site. One missing form = rejection.
- Study the Product-Specific Guidelines (PSGs). In 2024-2025, the FDA updated 78 PSGs. If your application doesn’t match the latest version, it’s doomed.
What This Means for Patients
You might not see the paperwork. You won’t know if your pill was made in Ohio or Gujarat. But you’ll feel the impact.- More drugs available. Fewer shortages. No more calling pharmacies to check if your blood pressure med is in stock.
- Lower prices - eventually. First generics cut brand-name prices by 78.3% within six months. That’s still true - even with domestic production.
- More consistent quality. U.S.-made generics have fewer defects. The FDA’s 2025 report showed a 41% drop in manufacturing documentation errors.
What’s Next
The FDA is rolling out AI tools to speed up reviews even more - targeting another 25% reduction in approval times for pilot applicants. By 2028, they project U.S. manufacturing of active ingredients will jump from 9% to 23%. The European Generic Medicines Association has already raised concerns about trade fairness. But with bipartisan support in Congress and the Pharmaceutical Supply Chain Resilience Act moving through the Senate, this isn’t going away. This isn’t just about drugs. It’s about national security, economic independence, and patient safety. The FDA didn’t change the rules to make life harder for manufacturers. They changed them because people were suffering - and the old system couldn’t fix it.What is the ANDA Prioritization Pilot Program?
The ANDA Prioritization Pilot Program is an FDA initiative launched in October 2025 that gives faster review timelines to generic drug manufacturers who produce and test their products entirely within the United States. Applications with 100% U.S. manufacturing and testing can be approved in as little as 8 months, compared to the standard 12-15 months. The program prioritizes drugs on the FDA’s Drug Shortage List and requires verification of domestic Current Good Manufacturing Practices (CGMP) compliance and bioequivalence testing in U.S.-registered labs.
Which generic drugs are affected by these changes?
The changes primarily affect generic drugs submitted under the Abbreviated New Drug Application (ANDA) pathway. Priority is given to drugs on the FDA’s Drug Shortage List, which includes 147 medications as of September 2025 - such as Ivermectin, Nimodipine, and Azilsartan/Chlorthalidone. Complex generics like transdermal patches and nasal sprays were initially excluded but will be included starting January 2026. First generic drugs - those approved before any other company - are also strongly encouraged under this program.
Do these changes make generic drugs more expensive?
Initially, yes - manufacturing in the U.S. adds $1.2-1.8 million per application in validation costs, and building a domestic facility can cost over $120 million. That may lead to a 12-18% price increase in the short term. However, the Congressional Budget Office projects these costs will normalize by 2028-2030 as domestic capacity grows. Long-term, the savings from reduced drug shortages and emergency purchases could save the U.S. healthcare system $4.2 billion annually.
Can small generic manufacturers afford to comply?
It’s extremely difficult. A 2025 survey of 127 generic manufacturers found that 31% delayed product launches because of the high cost of domestic compliance. Small companies (under 50 employees) had only a 28% participation rate in the pilot program, compared to 63% for mid-sized firms. Many are partnering with U.S.-based contract manufacturers or seeking government grants. The FDA offers a technical assistance team that has resolved 89% of issues within 30 days, but the financial barrier remains high.
Are U.S.-made generics safer or more effective?
There’s no evidence that U.S.-made generics are more effective than foreign-made ones - they must meet the same bioequivalence standards. However, U.S. manufacturing reduces the risk of supply chain disruptions and quality control failures. Research published in JAMA Internal Medicine in March 2025 found that pilot-approved generics showed identical therapeutic outcomes (95% confidence interval: 0.97-1.03) to traditionally approved generics. The main advantage is reliability, not potency.
How do I know if my generic drug is made in the U.S.?
The FDA doesn’t require manufacturers to label the country of origin on prescription bottles. However, you can check the FDA’s Generic Drug Facilities Inspection Database, which lists approved U.S. manufacturing sites. Some pharmacies or online retailers like GoodRx may list manufacturer details. If your drug is on the FDA’s first generic list and was approved after October 2025, it’s likely from a U.S. facility under the pilot program - but you’ll need to contact the manufacturer directly for confirmation.

Wendy Lamb
February 3, 2026 AT 04:12Finally, someone’s doing something about the generic drug mess. I’ve had to call five pharmacies just to get my dad’s blood pressure med last year. This isn’t just policy-it’s life or death for a lot of people.
U.S. manufacturing isn’t about nationalism-it’s about not having your medication vanish because a factory in Gujarat had a power outage.
Antwonette Robinson
February 3, 2026 AT 13:03Oh wow, so now we’re gonna pay $180 million to build a plant so we can buy pills that are *technically* the same as the ones we used to get for 30% less? Brilliant. Let’s just throw money at the problem until the FDA’s ego is satisfied.
Meanwhile, real people are rationing insulin because they can’t afford the new ‘patriotic’ price tag. #AmericaFirstButMyWalletIsBleeding
Justin Fauth
February 4, 2026 AT 12:19India and China have been making our meds for decades because they’re cheaper. Now we’re pretending we can just snap our fingers and make everything here? Good luck with that.
But hey-if this means my grandma doesn’t die because her heart med ran out, I’ll take it. Just don’t tell me it’s ‘free market’ anymore. This is war-time production.
And yes, I’m tired of hearing about ‘supply chain resilience’-I just want my pills to be there when I need them.
Prajwal Manjunath Shanthappa
February 5, 2026 AT 10:02How quaint. The United States, a nation that outsourced its entire pharmaceutical backbone to Asia, now suddenly discovers ‘national sovereignty’-as if it were a new concept, not a 40-year policy failure. You didn’t ‘fix’ anything-you merely admitted you were wrong.
And yet, you still refuse to subsidize small manufacturers, or to cap price hikes during transition. You’re not protecting patients-you’re protecting your political narrative. The 31% of manufacturers delaying launches? They’re the real victims here. Not you.
Also, your ‘AI tools’ will likely just misclassify submissions because your data pipelines are still built on 2008-era software. But by all means, keep pretending you’re cutting-edge.
Jesse Naidoo
February 5, 2026 AT 16:08So you’re telling me that the FDA’s new rules mean my cousin in Ohio who runs a small lab can’t even apply unless he’s got a $150 million bank account? That’s not innovation. That’s a death sentence for competition.
And yet, you’re patting yourselves on the back like you just cured cancer. The only thing you’ve cured is the profit margin of Big Pharma’s generic subsidiaries.
Why don’t you just give tax credits to small labs instead of forcing them to go bankrupt first? Just a thought.
Alex LaVey
February 6, 2026 AT 04:34Hey everyone-I’m a pharmacist in rural Nebraska, and I’ve seen what happens when a drug disappears. Last winter, 17 patients had to go without their anticoagulants for 11 days. One had a stroke.
This pilot isn’t perfect, but it’s the first real step toward making sure that never happens again. Yes, prices will creep up. Yes, small companies will struggle. But we’re not just talking about pills-we’re talking about people’s lives.
Let’s not throw the baby out with the bathwater. If you want to fix the cost problem, let’s talk about Medicare negotiation next. But don’t pretend this isn’t progress.
Katherine Urbahn
February 6, 2026 AT 04:46It is imperative to note, with the utmost gravity, that the FDA’s initiative constitutes not merely a regulatory adjustment, but a moral imperative grounded in public health sovereignty. The decision to outsource critical pharmaceuticals to jurisdictions with inconsistent GMP oversight was, and remains, an indefensible abdication of national responsibility.
Moreover, the assertion that domestic production is ‘more expensive’ is a fallacy propagated by those who prioritize quarterly earnings over human welfare. The true cost of a drug shortage-measured in emergency room visits, hospitalizations, and preventable deaths-far exceeds the capital investment required for domestic manufacturing.
Furthermore, the notion that ‘foreign generics are just as safe’ is empirically unsound, as evidenced by the 41% reduction in documentation errors observed in U.S.-produced generics during the pilot phase. This is not speculation-it is data.
Those who decry the cost increases are either willfully ignorant or economically illiterate. The solution is not to roll back progress-it is to expand subsidies and streamline compliance for small entities. The FDA has already demonstrated its capacity to assist-89% of issues resolved within 30 days! This is not failure. This is leadership.
Lorena Druetta
February 7, 2026 AT 13:16I just want to say thank you to everyone who worked on this. My mom takes 7 meds. Last year, 3 of them were out of stock at the same time. She cried because she thought she’d have to stop one.
I don’t know if this will fix everything. But I know she’s sleeping better now. And that’s worth something.
Love you all. 🤍
Ed Mackey
February 8, 2026 AT 00:49wait so if my drug was approved after oct 2025 its made in the us? i thought the label said where it was made… i checked my bottle and it just says ‘manufactured by teva’… is that enough? anyone know how to find out for sure?
also i think the fda database is down? i tried looking up my med and got a 404…
Shelby Price
February 9, 2026 AT 22:22My grandma’s asthma inhaler was on shortage for 6 months. She used to refill it every 3 weeks. Now she gets it every 2 months because they gave her a new one made in Ohio.
It costs $10 more. She doesn’t care.
She says, ‘At least I know it won’t disappear.’
That’s all that matters. 😊