Sick Day Medication Guide
Your Current Situation
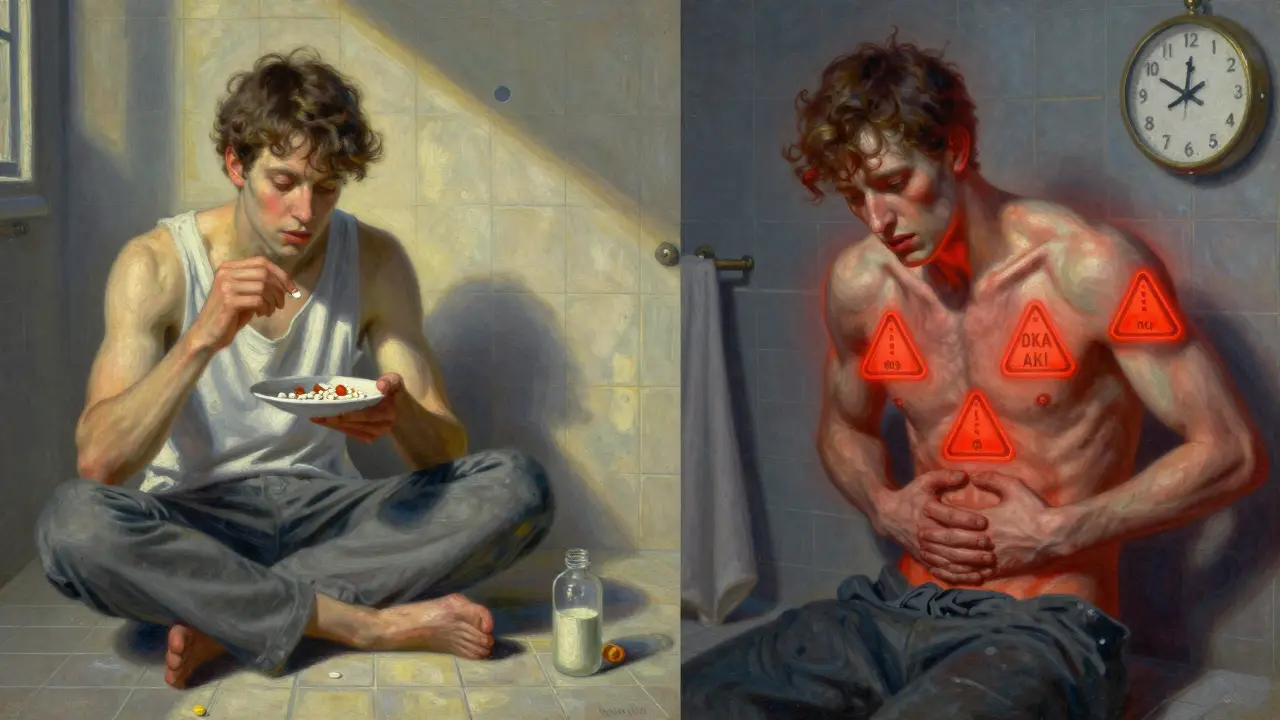
When you’re sick with a cold, flu, or stomach bug, your body is under stress. For someone with diabetes, that stress can turn a simple illness into a medical emergency. Diabetic ketoacidosis (DKA) and acute kidney injury (AKI) don’t wait for you to feel better-they can strike fast, especially if your diabetes meds aren’t adjusted properly. And here’s the scary part: diabetes medications that keep you stable on a normal day can become dangerous when you’re vomiting, feverish, or not drinking enough. This isn’t theory. It’s real. In 2023, over 1.2 million diabetes-related hospitalizations in the U.S. were linked to poor medication management during illness. Most of them were preventable.
Why Illness Changes Everything for Diabetes Medications
Your body doesn’t care if you’re feeling under the weather. When you’re sick, your liver dumps extra glucose into your bloodstream. Your muscles stop responding to insulin. Your kidneys work harder. And if you’re not eating or drinking, your blood sugar can swing wildly. That’s when your usual diabetes meds can backfire.
Take metformin. It’s safe for most people. But during illness, especially with vomiting or diarrhea, your kidneys can’t clear it properly. That raises your risk of lactic acidosis-a rare but deadly buildup of acid in your blood. Studies show the risk jumps 8.3 times when you’re dehydrated and your creatinine level rises above 1.5 mg/dL. That’s why stopping metformin at the first sign of sickness isn’t optional-it’s lifesaving.
Then there are SGLT2 inhibitors: drugs like empagliflozin, dapagliflozin, and canagliflozin. These help lower blood sugar by making your kidneys flush out glucose. Sounds good, right? But when you’re sick and not drinking enough, those same kidneys start burning fat for fuel. That leads to ketones. And ketones + SGLT2 inhibitors = euglycemic DKA. That’s diabetic ketoacidosis even when your blood sugar looks normal. The FDA reported a 7.2-fold increase in DKA cases tied to these drugs during illness. And the clock starts ticking the moment you feel nauseous.
Even blood pressure meds like ACE inhibitors and ARBs-lisinopril, losartan, valsartan-can hurt you when you’re sick. They protect your kidneys when you’re healthy. But when dehydration hits, they can cause your kidneys to shut down. A 2022 meta-analysis found a 40% spike in AKI risk when fluid intake drops below 1,500 mL per day. That’s less than six 12-ounce bottles of water. If you’re sipping tea and skipping meals, you’re already in danger.
What to Do When You’re Sick: The Medication Rules
There’s no one-size-fits-all plan. But here’s what the latest guidelines (ADA 2023, IDF 2022, NICE 2023) agree on:
- Stop metformin immediately if you’re vomiting, have diarrhea, or have a fever above 100.4°F (38°C). Don’t wait. Don’t think you’ll be fine. Restart only after you’ve eaten normally for 24 hours and your doctor says it’s safe.
- Stop SGLT2 inhibitors at the first sign of illness-even if you just have a headache or mild nausea. These drugs don’t wait. The FDA says: discontinue them immediately. Don’t wait 24 hours. That 300% increased DKA risk isn’t a suggestion-it’s a warning.
- Pause ACE inhibitors and ARBs if you’re drinking less than 1,500 mL (about 6 cups) of fluid in 24 hours. This includes soups, broths, and sugar-free drinks. If you’re only sipping water because you’re nauseous, stop these meds. Restart only after you’re eating, drinking, and your doctor clears you.
- Keep taking insulin-even if you’re not eating. This is critical. Type 1 patients need to increase their basal insulin by 10-20% every 4 hours if blood sugar is above 15 mmol/L (270 mg/dL). Type 2 patients on insulin may also need more. Studies show 68% of type 2 insulin users need higher doses when sick. Never skip insulin. Skipping it is how DKA starts.
- Keep sulfonylureas (like glimepiride) and DPP-4 inhibitors (like sitagliptin) unless you’re at risk of low blood sugar. These are safer than metformin during illness, but watch for hypoglycemia. If you’re not eating, you might need to reduce the dose.
And here’s the hard truth: not all doctors agree. One endocrinologist might tell you to keep metformin. Another will say stop it. The ADA says stop. The IDF says stop. NICE says stop. But Joslin Diabetes Center says, “Always take your meds unless your provider says otherwise.” That confusion is why 28% of patients don’t know what to do. If you’re unsure, err on the side of caution. Stop the risky meds. Call your provider.
Monitoring: What to Check and How Often
When you’re sick, checking your blood sugar isn’t enough. You need to check more-and check for ketones.
- Test blood sugar every 2 to 4 hours. That’s at least six times a day. Set alarms. Write it down. Use the ADA’s free Sick Day Log. Don’t guess. Don’t assume you’re fine because you feel okay.
- Test for ketones when your blood sugar is above 240 mg/dL (13.3 mmol/L). Use urine strips or a blood ketone meter. Urine ketones over 1.5 mmol/L or blood ketones over 0.6 mmol/L mean danger. Call your doctor or go to the ER. Don’t wait.
- Watch for signs of AKI. Reduced urine output, swelling in your legs, sudden fatigue, or confusion? These aren’t just “feeling bad.” These are your kidneys failing. AKI can happen fast-and it’s often silent until it’s too late.
- Target blood sugar range during illness: 100-180 mg/dL (5.6-10 mmol/L). Don’t chase perfection. Don’t let your blood sugar crash trying to hit normal numbers. Your body is fighting an infection. Stability is the goal.
Your Sick Day Kit: What to Have Ready
Waiting until you’re sick to prepare is too late. Build your kit now-before flu season hits.
- Glucose meter with 50+ test strips
- Ketone strips (urine or blood) - at least 10
- 7-day supply of all your medications (including insulin)
- 6 bottles of sugar-free fluids: water, broth, sugar-free electrolyte drinks (like Nuun or Pedialyte)
- Fast-acting carbs: juice boxes, glucose tablets, honey packets
- Simple snacks: crackers, applesauce, yogurt
- Written sick day plan from your doctor (yes, ask for one)
People who use these kits are 78% less likely to end up in the hospital. That’s not luck. That’s preparation.
When to Call for Help: Emergency Red Flags
You don’t need to wait until you’re collapsing. These are signs to call 999 or go to A&E immediately:
- Blood sugar below 70 mg/dL and doesn’t improve after 30g of fast-acting carbs
- Ketones above 1.5 mmol/L for more than 2 hours
- Vomiting for more than 4 hours
- Diarrhea for more than 6 hours
- Confusion, trouble breathing, fruity-smelling breath (sign of DKA)
- Little or no urine output for 12+ hours
These aren’t “maybe” situations. They’re emergencies. Delaying care can cost you your kidneys-or your life.

Why Guidelines Don’t Always Work-And What to Do About It
The guidelines are solid. But they’re not perfect. They were made for healthy adults. They don’t account for elderly patients with heart failure, kidney disease, or multiple meds. One study found 31% of older adults with diabetes still had medication-related complications even when they followed the rules.
And the advice? It’s inconsistent. One clinic says stop metformin. Another says keep it. A survey found 41% of patients got conflicting instructions from their GP and endocrinologist. That’s not your fault. It’s a system failure.
So here’s your action plan:
- Ask your doctor now: “What’s my sick day plan? Which meds do I stop, and when?” Get it in writing.
- Save your doctor’s number in your phone under “Diabetes Emergency.”
- Text or call them the moment you get sick-even if you think it’s just a cold.
- Don’t trust online advice. Trust your provider’s written plan.
And if you’re on a GLP-1 agonist like semaglutide? There’s no clear guidance yet. These drugs are new. The data is still coming. Until then, treat them like SGLT2 inhibitors: stop them if you’re vomiting or dehydrated. Better safe than sorry.
Final Thought: This Is About Survival, Not Perfection
Diabetes isn’t just about numbers. It’s about survival. When you’re sick, your body is fighting two battles: the infection, and the side effects of your own meds. The rules aren’t complicated. They’re simple: stop the risky drugs, keep insulin going, drink fluids, test often, and call for help early.
You don’t need to be a diabetes expert. You just need to be prepared. Build your kit. Know your plan. Don’t wait until you’re in the hospital to realize you should’ve stopped metformin three days ago.
Illness doesn’t wait. Neither should you.

Ian Ring
January 2, 2026 AT 12:02Just read this after my last hospital trip-thank you. I stopped metformin too late last time. Now I’ve got my sick-day kit ready: ketone strips, juice boxes, and a printed copy of this post taped to my fridge. I’m not risking it again. 😅
Angela Fisher
January 3, 2026 AT 06:02Wait… so you’re telling me the FDA, ADA, and Big Pharma are ALL lying about SGLT2 inhibitors? They’ve been pushing these drugs for YEARS while quietly knowing they cause DKA in sick people? I’ve been on dapagliflozin for 3 years. My doctor said it was ‘revolutionary.’ Now I’m wondering if my kidney damage was intentional. Who profits when diabetics end up in the ER? 🤔💸
Neela Sharma
January 5, 2026 AT 05:00This isn’t just medical advice-it’s a lifeline. When your body is screaming for help, your meds shouldn’t be the enemy. I used to think diabetes was about counting carbs. Now I know it’s about listening. To your body. To your fear. To your gut when something feels off. Stop the drugs. Drink water. Test. Call. That’s not weakness. That’s wisdom. 🌱💧
Palesa Makuru
January 6, 2026 AT 10:22Oh please. You think this is groundbreaking? I’ve been telling my patients for years that metformin is a ticking time bomb when they’re sick. But no one listens until they’re in the ICU. And don’t even get me started on how many people think ‘sugar-free electrolytes’ are just fancy Gatorade. Newsflash: Pedialyte isn’t a trend. It’s survival. 🙄
Lori Jackson
January 6, 2026 AT 17:26Per ADA 2023 guidelines, Section 7.4: ‘SGLT2 inhibitors are contraindicated during acute illness due to elevated euglycemic DKA risk.’ Also, NICE CG192 confirms. The real issue? Patients don’t have access to ketone meters. This isn’t negligence-it’s systemic underfunding of diabetic care. If you’re not testing blood AND ketones, you’re gambling with your nephrons. #DiabetesAwareness
Wren Hamley
January 7, 2026 AT 02:25So if I’m on a GLP-1 and get a stomach bug, do I stop it? Or just ride it out? I’ve seen zero papers on semaglutide + illness. My endo said ‘use your best judgment.’ But what’s ‘best’ when your blood sugar’s 180 and you’re throwing up? Also, why does no one talk about the fact that insulin doses need to be adjusted hourly during illness? That’s wild. I’m gonna start logging my temps and glucose every 90 mins. Maybe I’ll make a spreadsheet.
Sarah Little
January 8, 2026 AT 15:45My mom had AKI last winter because she kept her losartan. She didn’t drink enough water because she thought ‘drinking more’ meant ‘more sugar.’ She’s fine now but I’m still mad. Why isn’t this in every doctor’s office? Why is this knowledge only on Reddit? 🤷♀️
innocent massawe
January 9, 2026 AT 21:12I live in Nigeria. We don’t have ketone strips. We don’t have easy access to insulin. But we still get sick. This post made me cry. My sister has type 1. I just wrote down the rules in my notebook. If she gets fever, I stop metformin. I give her water. I call the clinic. That’s all we can do. Thank you for writing this. 🙏
veronica guillen giles
January 11, 2026 AT 12:45Wow. A diabetes post that doesn’t end with ‘just lose weight.’ Who knew? 😏 Honestly, this is the most useful thing I’ve read all year. I’m printing it. I’m laminating it. I’m sending it to my cousin who thinks ‘diabetes meds are like vitamins.’ Spoiler: they’re not. Thanks for not sugarcoating it. (Pun intended.)
Tru Vista
January 12, 2026 AT 12:39Stop metformin? Really? My doc says keep it. I think you’re overreacting. Also, typo in ‘diarrhea’ lol.