When you take two drugs at the same time, it’s not just about what each one does alone. Sometimes, they team up in ways that can be life-saving-or life-threatening. This isn’t about one drug changing how the other is absorbed or broken down in your body. That’s pharmacokinetics. This is about what happens when drugs meet at the target site: your cells, your receptors, your organs. This is pharmacodynamic drug interactions.
What Exactly Is a Pharmacodynamic Interaction?
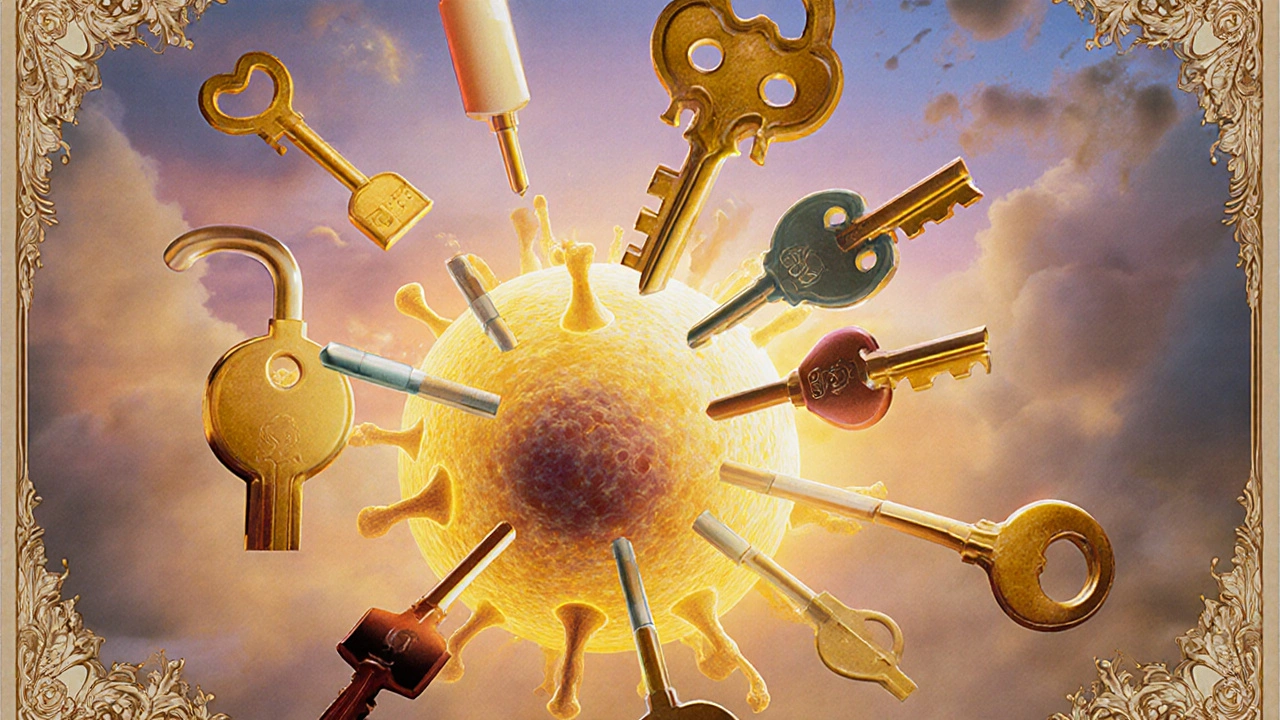
Imagine your body has thousands of locks (receptors), and drugs are keys. A pharmacodynamic interaction happens when one key changes how another key fits-or even blocks it-without touching the lock itself. The concentration of the drugs stays the same, but their effect doesn’t. One drug can make another stronger, weaker, or even reverse its action.
This isn’t theoretical. In hospital settings, about 40% of serious drug interactions are pharmacodynamic, according to data from European teaching hospitals between 2015 and 2017. And unlike pharmacokinetic interactions-where you can often fix the problem by lowering a dose-these are trickier. You can’t just reduce the amount. Sometimes, you have to stop one drug entirely.
Three Ways Drugs Can Interact at the Target Level
Pharmacodynamic interactions fall into three clear categories: synergistic, additive, and antagonistic. Each has real-world consequences.
- Synergistic: The combined effect is greater than the sum of the parts. Think of trimethoprim and sulfamethoxazole. Together, they block two steps in bacterial folic acid production. Alone, each needs a high dose. Together, they work better at 75% less of each. This is why it’s one of the most common antibiotic combos.
- Additive: The total effect equals the sum of each drug’s individual effect. Taking two painkillers like acetaminophen and ibuprofen together for a headache often works this way. It’s predictable, and often intentional.
- Antagonistic: One drug blocks or reduces the effect of another. This is where things get dangerous. For example, if you’re on albuterol for asthma and your doctor prescribes propranolol for high blood pressure, you’re at risk. Propranolol blocks the same beta-2 receptors that albuterol needs to open your airways. The result? Your asthma could worsen-or stop responding entirely.
Receptor-Level Battles: Who Wins the Lock?
Many of these interactions happen at the receptor level. Drugs don’t just bind to receptors-they compete for them. The winner depends on two things: affinity and efficacy.
Affinity is how tightly a drug sticks to its target. Potency (EC50) tells you how little of it you need to get a response. Efficacy (Emax) is how strong the response can be. If Drug A has higher affinity than Drug B, it’ll crowd out Drug B-even if Drug B is given in a higher dose.
Take opioid drugs. Morphine activates opioid receptors to relieve pain. Naloxone, used to reverse overdoses, has even higher affinity. It kicks morphine off the receptor, instantly reversing its effects. In someone dependent on opioids, this doesn’t just stop pain-it triggers full-blown withdrawal. That’s why naloxone is given carefully.
Physiological Interference: When Drugs Fight Behind the Scenes
Not all interactions happen at the same receptor. Sometimes, drugs interfere with the body’s own systems.
Take NSAIDs like ibuprofen and ACE inhibitors like lisinopril. ACE inhibitors lower blood pressure by relaxing blood vessels and helping the kidneys remove salt and water. But NSAIDs block prostaglandins-chemicals that help keep blood flowing to the kidneys. When you take them together, the kidneys get less blood flow. Studies show this drops renal blood flow by about 25%. The result? Blood pressure doesn’t drop as it should. In older patients, this combo can even lead to sudden kidney failure.
Another example: diuretics (water pills) and NSAIDs. The diuretic tells your body to pee out salt and water. The NSAID tells your kidneys to hold onto it. The diuretic stops working. This is why doctors warn against mixing these, especially in people with heart failure or high blood pressure.

The Most Dangerous Combinations
Some pharmacodynamic interactions aren’t just risky-they’re deadly.
- SSRIs + MAOIs: Mixing antidepressants like sertraline with MAOIs like phenelzine can cause serotonin syndrome. Your body floods with serotonin. Symptoms: high fever, seizures, muscle rigidity, confusion. A 2021 meta-analysis found this combo increases serotonin syndrome risk by 24 times. It’s rare-but fatal in up to 20% of cases.
- Opioids + benzodiazepines: Both depress the central nervous system. Together, they slow breathing to dangerous levels. The FDA issued a black box warning in 2016 after thousands of overdose deaths linked to this combo.
- Anticoagulants + antiplatelets: Warfarin and aspirin together can cause uncontrolled bleeding. A 2022 survey of UK doctors found this was the most common dangerous interaction they saw monthly.
These aren’t edge cases. They’re routine mistakes. In one Reddit thread from a hospital pharmacist, a patient on linezolid (an antibiotic) and sertraline (an antidepressant) developed serotonin syndrome and spent three days in intensive care. Neither drug alone would have caused it. Together? Catastrophic.
When Interactions Are a Good Thing
Not all pharmacodynamic interactions are bad. Medicine uses them on purpose.
Low-dose naltrexone, once used only for addiction, is now being studied with antidepressants. In a 2021 trial with 142 patients, this combo improved treatment-resistant depression in 68% of cases-compared to just 42% with antidepressants alone. Naltrexone blocks opioid receptors briefly, triggering the body to produce more natural painkillers and mood boosters. It’s a clever hack of the body’s own systems.
Another example: combining levodopa with carbidopa in Parkinson’s. Carbidopa doesn’t cross the blood-brain barrier. It stops levodopa from breaking down in the gut and bloodstream, so more reaches the brain. The result? Lower doses, fewer side effects, better control.
Who’s at Highest Risk?
People taking five or more medications are 10 times more likely to have a dangerous interaction. That’s why older adults are the most vulnerable. The average 70-year-old in the UK takes 4.8 prescriptions. By 2050, 1.5 billion people worldwide will be over 65.
But it’s not just age. People with chronic conditions-diabetes, heart disease, depression-are often on multiple drugs. A 2019 NIH study found that 83% of life-threatening pharmacodynamic interactions involved at least one drug with a narrow therapeutic index. That means the difference between a helpful dose and a toxic one is tiny. Warfarin, digoxin, lithium, and some anti-seizure drugs fall into this category.

How Doctors and Pharmacies Try to Stop These Interactions
Electronic health records now flag potential interactions. But they’re not perfect. A 2020 study found they miss 22% of serious pharmacodynamic interactions because they’re programmed to look for obvious combos-like SSRIs and MAOIs-but miss subtler ones, like NSAIDs reducing the effect of blood pressure drugs.
The most effective defense? Pharmacist-led medication reviews. A 2021 review in BMJ Quality & Safety showed that when pharmacists sit down with elderly patients to review every pill they take, adverse events drop by 58%. The top two interactions they caught? NSAIDs with blood pressure meds, and anticoagulants with antiplatelets.
Tools like the University of Liverpool’s HIV Drug Interactions database are widely used by specialists, but they don’t cover everything. Newer systems, like the one being piloted by the NHS in 12 UK hospitals, aim to link real-time patient data with interaction databases to give alerts before the prescription is even written.
What You Can Do
You don’t need to be a doctor to protect yourself.
- Keep a list of every medication you take-including supplements, vitamins, and over-the-counter painkillers.
- Bring that list to every appointment. Don’t assume your doctor knows what you’re taking.
- Ask: “Could this new medication interact with anything else I’m on?”
- If you feel strange after starting a new drug-dizziness, confusion, rapid heartbeat, trouble breathing-call your doctor immediately. Don’t wait.
Pharmacodynamic interactions aren’t always obvious. But they’re predictable. And with the right questions, you can avoid the worst outcomes.
What’s Next for Drug Interaction Science?
Researchers are building smarter tools. Dr. Rada Savic’s team at UCSF used machine learning to predict serotonin syndrome risk with 89% accuracy by analyzing patient data, drug doses, and genetic factors. The European Clinical Research Infrastructure Network just launched a $4.7 million database focused solely on pharmacodynamic interactions.
The goal isn’t just to warn doctors after the fact. It’s to prevent interactions before they happen-using AI, real-time data, and personalized medicine. In the future, your electronic health record might not just say “warning: possible interaction.” It might say, “Based on your age, kidney function, and current meds, adding ibuprofen increases your risk of acute kidney injury by 37%.”
That’s the future. But right now, the best tool you have is awareness-and asking the right questions.
What’s the difference between pharmacodynamic and pharmacokinetic drug interactions?
Pharmacokinetic interactions affect how your body absorbs, breaks down, or removes a drug-like when one drug blocks the liver enzyme that metabolizes another. Pharmacodynamic interactions happen at the target site: drugs change how each other works at receptors or in body systems, even if their levels in the blood stay the same. One changes the drug’s journey; the other changes its effect.
Can over-the-counter drugs cause pharmacodynamic interactions?
Absolutely. Common OTC drugs like ibuprofen, aspirin, and even antihistamines can interfere with prescription medications. Ibuprofen can block the effect of blood pressure drugs. Antihistamines like diphenhydramine can add to the sedation of opioids or benzodiazepines. Always check with your pharmacist before mixing any new OTC product with your regular meds.
Why are pharmacodynamic interactions harder to predict than pharmacokinetic ones?
Pharmacokinetic interactions follow clear chemical rules-you can measure enzyme activity, blood levels, and half-lives. Pharmacodynamic interactions depend on complex biology: receptor density, tissue sensitivity, disease state, and even genetics. Two people on the same drugs might react completely differently. That’s why clinical judgment and patient monitoring matter more than algorithms alone.
Are herbal supplements safe to take with prescription drugs?
Not necessarily. St. John’s wort can reduce the effectiveness of birth control, antidepressants, and blood thinners by altering receptor activity. Garlic and ginkgo can increase bleeding risk when taken with warfarin or aspirin. Many people assume “natural” means safe, but herbs are potent chemicals that interact with your body just like drugs do.
How can I know if I’m experiencing a pharmacodynamic interaction?
Watch for sudden changes after starting a new drug: your blood pressure isn’t dropping, your asthma is getting worse, you’re unusually drowsy, or you’re bleeding more easily. If something feels off-especially if it’s new and you’ve changed your meds-contact your doctor. Don’t assume it’s just “side effects.” It could be an interaction.
Johnson Abraham
November 13, 2025 AT 20:08Shante Ajadeen
November 14, 2025 AT 10:57dace yates
November 16, 2025 AT 09:40Danae Miley
November 17, 2025 AT 13:12Erica Cruz
November 18, 2025 AT 07:42And don’t even get me started on the 78-year-old on lisinopril and ibuprofen for ‘arthritis’ who ended up in dialysis. These aren’t edge cases-they’re Tuesday.
Renee Ruth
November 19, 2025 AT 01:38Someone needs to sue the entire pharmaceutical-industrial complex.
Samantha Wade
November 20, 2025 AT 13:58And yes, OTC drugs are not ‘harmless.’ The FDA’s own data shows OTC-related ED visits have doubled since 2010. Stop normalizing polypharmacy.
Elizabeth Buján
November 22, 2025 AT 11:35my dad’s on 8 meds. he doesn’t even know what half of them do. i started keeping a little notebook for him. just names, doses, and why. it’s tiny. but it’s something.
we don’t need more tech. we need more patience. more listening. more care.
Andrew Forthmuller
November 23, 2025 AT 02:32Charles Lewis
November 24, 2025 AT 02:28Therefore, while AI-driven alert systems are promising, their efficacy is contingent upon patient engagement, health literacy, and provider-patient communication dynamics. The most sophisticated algorithm cannot compensate for a patient who does not understand why they are being warned against ibuprofen.
Thus, the solution lies not solely in technological innovation, but in cultivating a culture of collaborative, empathetic, and linguistically accessible care. We must educate not only clinicians, but the public-starting in high school biology curricula. Pharmacodynamics is not a specialty; it is a civic responsibility.