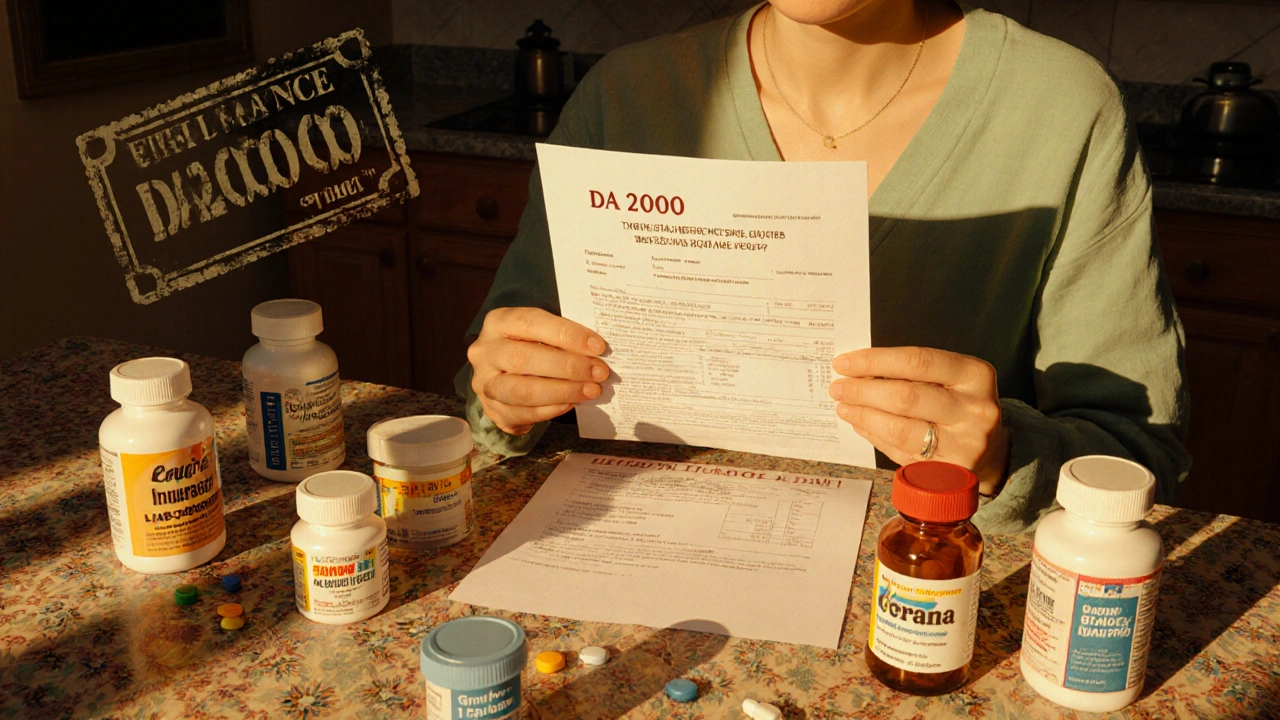
Insurance Appeal: How to Fight Denied Medication Claims and Get Coverage
When your insurance appeal, a formal request to overturn a denied medication claim. Also known as pharmacy dispute, it’s your right to challenge a decision that blocks access to essential drugs. Many people give up after their insurer says no—but that’s often the first step, not the final word. A well-structured appeal can get you the medication your doctor prescribed, whether it’s for diabetes, high blood pressure, or mental health. You don’t need a lawyer. You just need to know what to say and what papers to send.
Insurance companies deny prescriptions for all kinds of reasons: the drug isn’t on their formulary, they want you to try a cheaper alternative first, or they claim it’s "not medically necessary." But if your doctor says you need it, and your medical records back that up, you have a real shot at winning. medication denial, when an insurer refuses to pay for a prescribed drug. Also known as prior authorization rejection, it’s common—but not inevitable. The key is acting fast. Most insurers give you 60 to 180 days to appeal. Don’t wait. Gather your doctor’s letter, lab results, and any prior treatment records. If you’re on a chronic condition like rheumatoid arthritis or bipolar disorder, your history matters. Show them why the denied drug works better for you than the one they’re pushing.
Some appeals fail because people send generic templates. Others fail because they don’t include the right paperwork. Your doctor’s note isn’t enough—it needs to explain why alternatives failed, or why the specific drug is critical. For example, if you’re on warfarin and cranberry juice interactions make other blood thinners risky, that’s a documented medical reason. Or if you’ve tried three generics for depression and they all caused side effects, that’s data. prescription coverage, the portion of your drug cost your insurance agrees to pay. Also known as formulary access, it’s not a guarantee—it’s a negotiation. You’re not asking for a favor. You’re enforcing your rights under the Affordable Care Act and your plan’s own terms. And if your first appeal gets denied? There’s a second level. And a third. Many people win on appeal #2.
Look at the posts below. You’ll find real stories from people who fought back—like the parent who got coverage for a child’s rare epilepsy drug after proving insurance’s preferred option caused seizures. Or the senior who beat a denial for a generic blood pressure med because their kidney function made other drugs unsafe. These aren’t rare cases. They’re everyday battles with a clear path to victory. The system isn’t perfect, but it’s not closed either. You have tools. You have rights. And now you know how to use them.
When a generic medication fails to work for you, insurance denials can be frustrating - but not unbeatable. Learn how to fight back with medical evidence, step-by-step appeals, and proven strategies that work.
Read More