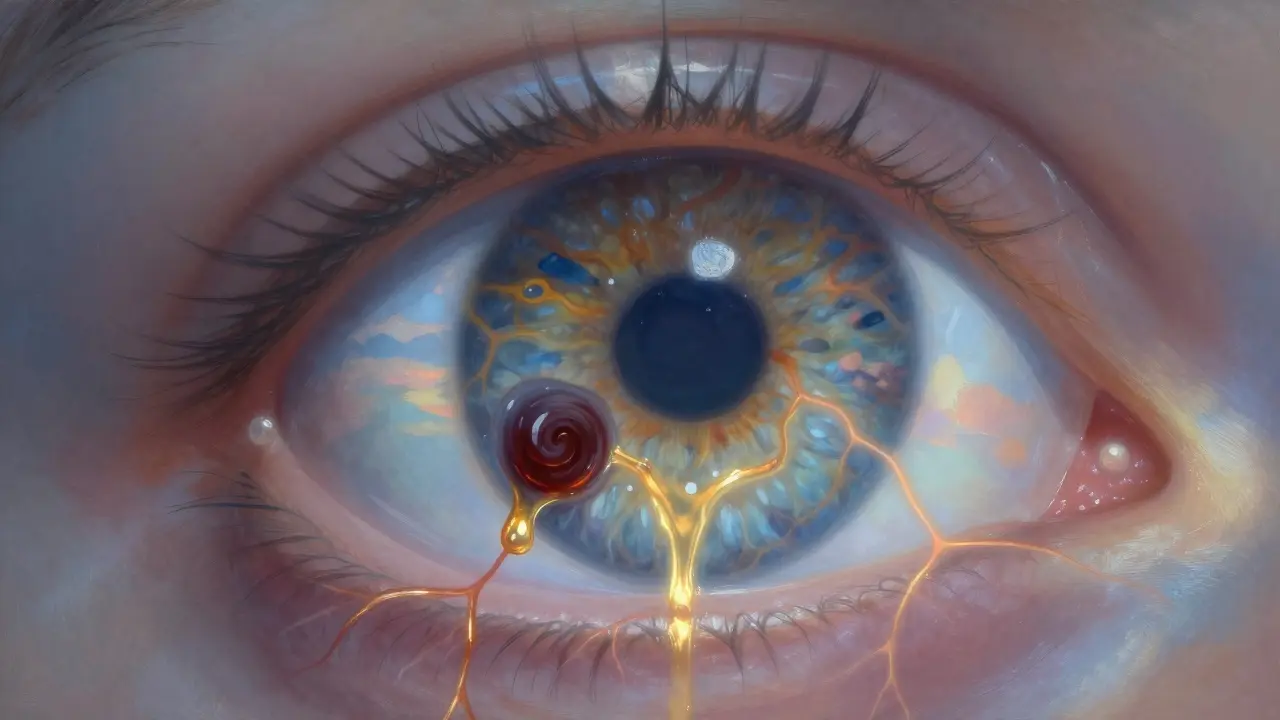
What Is Retinal Vein Occlusion?
Retinal vein occlusion (RVO) happens when a vein in the retina gets blocked, stopping blood from flowing out. The retina is the light-sensitive layer at the back of your eye. When it can’t drain properly, fluid leaks, blood builds up, and vision gets blurry or lost-sometimes suddenly and without pain. There are two main types: central retinal vein occlusion (CRVO), which affects the main vein, and branch retinal vein occlusion (BRVO), which hits smaller branches. CRVO is more serious and often causes worse vision loss. BRVO usually affects only part of your vision, like a dark spot in one corner.
Who Is at Risk for Retinal Vein Occlusion?
Most people who get RVO are over 65. About half of all cases happen in this age group. But it’s not just about getting older. Several health conditions make it much more likely.
Hypertension is the biggest risk factor. Up to 73% of people over 50 with CRVO have high blood pressure. Even if it’s been controlled for years, a sudden spike can trigger a blockage. Uncontrolled hypertension is especially dangerous for BRVO.
Diabetes shows up in about 10% of RVO cases over 50. It doesn’t cause the blockage directly, but it weakens blood vessels over time, making them more prone to clotting. People with diabetes also tend to have worse outcomes after RVO.
High cholesterol is another major player. If your total cholesterol is above 6.5 mmol/L, your risk jumps. This leads to fatty deposits in the walls of your arteries, which can press on nearby veins and crush them shut.
Glaucoma also increases risk, especially if pressure inside the eye is high. The optic nerve area is where veins often get pinched-so if you already have glaucoma, you’re more likely to get RVO right there.
Lifestyle factors matter too. Smoking is linked to 25-30% of cases. It thickens the blood and damages blood vessel walls. Obesity and being inactive contribute by raising blood pressure and cholesterol. Even if you’re young, these habits can set the stage for RVO later.
For women under 45, oral contraceptives are a known trigger, especially for CRVO. Blood clots form more easily with hormonal birth control. If you’ve had a blood clot before or have a family history of clotting disorders, this risk is even higher.
Less common but serious: blood disorders like polycythemia vera, multiple myeloma, or inherited clotting problems like factor V Leiden. These are rare but important to check for, especially if RVO happens before age 45.
How Is RVO Diagnosed?
If you suddenly lose vision or notice blurry spots, you need an eye doctor right away. No home remedy fixes this. The diagnosis starts with a basic eye exam, but the real clues come from special tests.
Optical coherence tomography (OCT) is the gold standard. It creates a detailed cross-section of your retina and shows exactly how much fluid has leaked into the macula-the center of your vision. If the central subfield thickness is over 300 micrometers, treatment is usually needed.
Fluorescein angiography involves injecting a dye into your arm and taking photos as it flows through the eye. This shows where the vein is blocked and how badly the blood flow is disrupted.
Doctors also check your blood pressure, run blood tests for cholesterol and glucose, and may ask about your medical history-especially if you’re under 50. The goal isn’t just to treat the eye; it’s to find what’s causing the blockage so you can prevent another one.

What Are the Main Injection Treatments?
There’s no way to unblock the vein. Treatment focuses on stopping the damage it causes-mainly macular edema, the swelling that blurs your vision.
The two main types of injections are anti-VEGF drugs and corticosteroids.
Anti-VEGF injections include ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin). These block a protein called VEGF that causes blood vessels to leak. They’re the first-line treatment for most patients. In clinical trials, patients gained 16-18 letters on the eye chart after 6 months of monthly shots. That’s the difference between barely reading a sign and reading it clearly.
Corticosteroid injections, like the dexamethasone implant (Ozurdex), reduce swelling and inflammation. They’re slower to work but last longer-up to 6 months. They’re often used when anti-VEGF doesn’t help enough, or for patients who can’t handle frequent injections.
Bevacizumab is used off-label because it’s much cheaper-about $50 per dose versus $2,000 for Lucentis or Eylea. In safety-net clinics, 60-70% of RVO injections are bevacizumab. In private practices, it’s closer to 30%. The results are similar, but insurance coverage varies.
What Does Treatment Actually Look Like?
Treatment isn’t a one-time fix. It’s a long-term commitment.
Most patients start with monthly injections for 3-6 months. After that, doctors switch to a treat-and-extend approach: if your eye stays stable, you wait 6 weeks, then 8, then 10, and so on. The goal is to space out shots as much as possible without losing vision. Studies show this cuts injection frequency by 30% with no drop in results.
On average, patients need 8-12 injections in the first year. Some need more. Others stabilize after 5-6. Your eye’s response is tracked with OCT scans every 4-8 weeks. If the swelling goes down below 250 micrometers, you’re on track.
The injection itself takes less than 10 minutes. Your eye is numbed with drops. The doctor cleans your eyelid with antiseptic, holds your eye open with a speculum, and gives a quick pinch-like injection near the white of your eye. You might see floaters or have a red spot afterward-common and harmless. Serious infections like endophthalmitis happen in fewer than 1 in 1,000 cases.
What Are the Downsides of Injections?
They work-but they come with trade-offs.
Cost is a huge barrier. Even with insurance, copays can hit $100-$150 per shot. For 12 shots a year, that’s $1,200-$1,800 out of pocket. Ozurdex implants cost $2,500 each but last longer. Many patients skip appointments because they can’t afford it.
Treatment fatigue is real. A survey of over 1,200 RVO patients found 41% stopped going to appointments because they were exhausted by the routine. The anxiety before each shot is often worse than the pain. One patient described it as “waiting for the hammer to drop.”
Steroid side effects include cataracts (60-70% of patients develop them within a year) and increased eye pressure (30% need drops to lower it). These are serious, especially if you’re young and still have your natural lens.
Anti-VEGF drugs are safer long-term, but they don’t work for everyone. About 1 in 5 patients don’t respond well, even after 6 months. That’s when doctors consider switching to steroids or combining both.
What’s New in RVO Treatment?
The future is about reducing burden and personalizing care.
One big development is the Port Delivery System (Susvimo), a tiny implant that slowly releases ranibizumab for up to 6 months. It’s already approved for wet AMD and is now being tested for RVO. If it works, it could cut injections from monthly to twice a year.
Gene therapy is on the horizon. RGX-314, currently in trials, aims to give your eye the ability to make its own anti-VEGF protein. One treatment could last years.
Another new drug, OPT-302, blocks a different VEGF protein (VEGF-C/D) and is being tested alongside aflibercept. Early results suggest it helps patients who didn’t respond to standard therapy.
Doctors are also using optical coherence tomography angiography (OCTA) to see blood flow in real time. This helps predict who will respond to which treatment before they even start.
What Can You Do to Prevent RVO?
If you’re over 50, or have diabetes, high blood pressure, or high cholesterol, you can lower your risk.
- Keep your blood pressure under 130/80
- Manage your blood sugar if you have diabetes
- Lower cholesterol with diet, exercise, and medication if needed
- Quit smoking-even cutting back helps
- Stay active. Walking 30 minutes a day improves circulation
- Get annual eye exams. RVO often has no warning signs until it’s too late
For younger people on birth control, talk to your doctor about clotting risks. If you’ve had unexplained clots in your legs or lungs, ask for a blood test for clotting disorders.
What’s the Long-Term Outlook?
With treatment, 30-40% of patients regain vision to 20/40 or better-that’s good enough to drive and read without magnifiers. Without treatment, most lose vision permanently.
But vision isn’t the only thing at stake. RVO is a warning sign. People who have it are 2-3 times more likely to have a stroke or heart attack in the next 5 years. That’s why managing your overall vascular health is just as important as treating your eye.
The goal isn’t just to see better-it’s to live longer. RVO isn’t just an eye disease. It’s a sign your whole body’s blood vessels are under stress.
Can retinal vein occlusion be cured?
No, there’s no cure for the blocked vein itself. But treatments like anti-VEGF injections can stop the swelling and fluid buildup that cause vision loss. Most patients stabilize or improve significantly with ongoing treatment. The key is early diagnosis and consistent follow-up.
How often do you need injections for RVO?
Most patients start with monthly injections for 3-6 months. After that, doctors use a treat-and-extend approach, gradually spacing shots out to every 6-12 weeks. On average, people need 8-12 injections in the first year. Some need fewer; others need more. The goal is to use the fewest injections possible while keeping vision stable.
Are eye injections painful?
The injection feels like a quick pinch or pressure. Numbing drops are used, so you won’t feel sharp pain. Some people report a gritty feeling or floaters afterward, which fades within hours. The anxiety before the injection is often worse than the procedure itself. Most patients get used to it after a few visits.
Can I drive after an RVO injection?
You shouldn’t drive the same day. Your pupil will be dilated, and your vision may be blurry or sensitive to light for a few hours. It’s best to arrange a ride home. Most people can drive again the next day, but check with your doctor if you’re unsure.
What happens if I miss an injection?
Missing one appointment won’t cause sudden blindness, but it increases the risk of fluid building up again. Vision can start to blur within weeks. If you miss a shot, call your doctor right away. They may reschedule you sooner or adjust your treatment plan. Consistency is key-this is a chronic condition that needs ongoing care.
Is Avastin safe for RVO?
Yes. Avastin (bevacizumab) is not officially approved for eye use, but decades of research and millions of injections show it’s as safe and effective as Lucentis or Eylea for RVO. It’s widely used, especially where cost is a concern. The risk of complications is the same as with branded drugs. The only difference is price-Avastin costs about $50 per dose.
Can RVO happen in both eyes?
It’s rare, but possible. About 5-10% of patients develop RVO in the other eye within 5 years. That’s why managing your overall health-blood pressure, cholesterol, diabetes-is so important. If you’ve had it in one eye, you’re at higher risk for it in the other.
Do I need to see a specialist for RVO?
Yes. While your regular eye doctor can diagnose RVO, treatment with injections requires a retina specialist. These doctors have advanced training in managing complex retinal diseases and use the latest imaging and injection techniques. Don’t delay-seeing a specialist within days of symptoms improves outcomes.
Aditya Kumar
December 15, 2025 AT 11:57Dan Padgett
December 16, 2025 AT 18:48Cassandra Collins
December 17, 2025 AT 18:18Andrew Sychev
December 19, 2025 AT 01:17Tiffany Machelski
December 19, 2025 AT 14:12James Rayner
December 20, 2025 AT 00:19Souhardya Paul
December 20, 2025 AT 17:41Josias Ariel Mahlangu
December 21, 2025 AT 00:58anthony epps
December 21, 2025 AT 01:05Hadi Santoso
December 22, 2025 AT 20:51Kim Hines
December 24, 2025 AT 18:52