Every year, hundreds of thousands of people end up in emergency rooms because of unexpected reactions between the medicines they’re taking. It’s not always a mistake by a doctor or pharmacist. Sometimes, it’s something as simple as taking ibuprofen with blood pressure pills, or mixing St. John’s Wort with an antidepressant - and not knowing until it’s too late. The good news? You don’t need to wait for a hospital visit to catch these dangers. With the right tools and a little caution, you can check for drug interactions at home - safely and effectively.
Why Drug Interactions Are More Common Than You Think
Most people don’t realize how many different substances they’re taking. It’s not just prescription pills. It’s the painkiller you grab for a headache, the magnesium supplement you started for sleep, the turmeric capsule your friend swore by, even grapefruit juice with your cholesterol med. According to the CDC, nearly 40% of Americans over 65 take five or more medications daily. That’s a recipe for hidden clashes. Drug interactions fall into three main types: drug-drug (61% of cases), drug-food/drink (27%), and drug-condition (12%). A major interaction can cause serious harm - think irregular heartbeat, kidney damage, or serotonin syndrome. Moderate ones might make you dizzy or nauseous. Minor ones? Usually just a nuisance. But you won’t know unless you check.How Drug Interaction Checkers Work
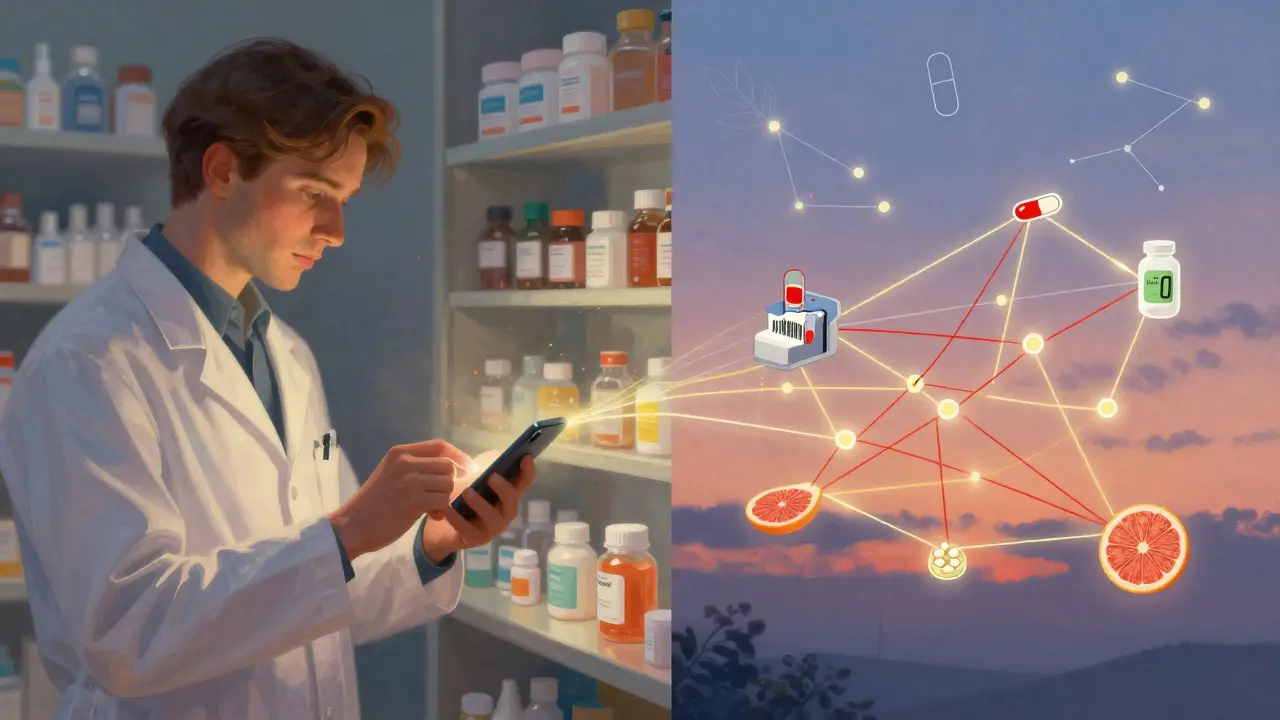
These tools aren’t magic. They’re databases built over decades using real-world clinical data. When you type in your meds - say, lisinopril, metformin, and a multivitamin - the checker compares each ingredient against a list of over 80,000 known interactions. It doesn’t guess. It matches chemical names, dosages, and how your body processes them. The big players are Drugs.com, WebMD, and Medscape. Drugs.com has the most complete database, covering 24,000 prescription drugs and 3,000 supplements. WebMD is easier to use, with color-coded warnings (red = major, yellow = moderate, green = minor). Medscape is powerful but designed for doctors - it’s harder for everyday users. These tools update constantly. Drugs.com refreshes daily. WebMD added 1,200 new supplement interactions in July 2023. And now, some use AI to predict how severe a reaction might be based on your age, weight, and other health factors.Step-by-Step: How to Check Your Meds at Home
You can do this in under 10 minutes. Here’s how:- Write down everything you take. Not just prescriptions. Include every OTC pill, vitamin, herb, and even occasional use - like aspirin before a flight or antacids after spicy food. Write the brand name, generic name, dose, and how often you take it. Example: Advil 200mg, ibuprofen, 1 tablet every 6 hours as needed for pain.
- Use a trusted checker. Go to Drugs.com or WebMD and find their free interaction checker. Avoid random apps you find in app stores - the FDA warned about 17 fake ones in 2022.
- Enter each item one at a time. Don’t rush. If you’re unsure about a supplement, search its active ingredient. For example, “ashwagandha” not “Nature’s Bounty Ashwagandha.” Many users miss this step and get false negatives.
- Read the results carefully. Look for red flags. A major interaction doesn’t mean you must stop the drug - it means you need to talk to your pharmacist or doctor immediately. Moderate ones might need a dose change. Minor ones? Often just a note to watch for dizziness or stomach upset.
- Print or save the report. Bring it to your next appointment. Don’t rely on memory. Pharmacists say 70% of patients forget half their meds during visits.
What These Tools Can’t Do
No digital tool is perfect. They miss rare interactions - especially with brand-new drugs or complex combinations. A 2023 Medscape case report showed a cancer drug interaction that no consumer checker caught. And they can give false positives. About 18% of alerts turn out to be harmless when reviewed by a professional. They also don’t know your full medical history. If you have kidney disease, liver issues, or are pregnant, that changes everything. A drug that’s safe for most people could be dangerous for you. That’s why experts like Dr. Michael Cohen from the Institute for Safe Medication Practices say these tools are a first step - not the final word. They’re meant to spark a conversation with your pharmacist, not replace it.Real Stories: When It Saved a Life
In 2022, a 68-year-old woman in Ohio was taking sertraline (Zoloft) for depression and daily St. John’s Wort for mood support. She didn’t think it was a problem - both were “natural.” But the Drugs.com checker flagged a major interaction: risk of serotonin syndrome, which can cause seizures, high fever, and even death. She showed the report to her doctor, who switched her to a different antidepressant. She’s still doing well today. Another user on Reddit, u/MedSafetyNurse, caught a dangerous interaction between warfarin and ibuprofen that her own doctor had missed. She stopped the ibuprofen and switched to acetaminophen - avoiding a potentially life-threatening bleed. But there are failures too. Some people panic and quit essential meds after seeing a yellow alert. The FDA says 15% of patients stop critical drugs like blood thinners or heart meds after a non-critical warning. That’s just as dangerous as ignoring the alert.Pro Tips for Safer Home Checking
- Use one pharmacy. Filling all your prescriptions at the same place cuts interaction risks by 31%. Pharmacists see your full history and can flag clashes before you even leave the store. - Scan barcodes. Apps like Medisafe let you scan the barcode on your pill bottle. It auto-fills the name, dose, and frequency. Saves time and reduces typos. - Check every 30 days. Your meds change. New prescriptions, seasonal supplements, even a different brand of painkiller - update your list regularly. - Know the warning signs. If you suddenly feel dizzy, confused, have a rapid heartbeat, or unexplained bruising after starting a new med - don’t wait. Call your doctor or go to urgent care. - Ask your pharmacist. They’re medication experts - not just pill dispensers. Most offer free 10-minute consultations. Use them.
What’s Coming Next
The future of drug safety is personal. By late 2024, GoodRx and 23andMe plan to launch pharmacogenomic screening - checking your DNA to see how your body breaks down certain drugs. Imagine knowing before you even start a medication whether it’ll cause side effects or not. By 2024, Medicare plans to integrate interaction checkers directly into MyMedicare accounts, so seniors get alerts right in their portal. Hospitals are already using these tools behind the scenes - Epic Systems now automatically screens prescriptions in 78% of U.S. hospitals. But the core truth won’t change: technology helps, but human expertise saves lives.Frequently Asked Questions
Can I trust free drug interaction checkers?
Yes - but only if they’re from trusted sources like Drugs.com, WebMD, or Medscape. Avoid apps you download from unknown developers. The FDA has flagged 17 fake interaction checkers since 2022. Stick to well-known medical websites with clear updates and citations.
Do I need to check interactions even if my doctor prescribed everything?
Absolutely. Doctors often prescribe one med at a time and may not know about every supplement or OTC drug you’re taking. A 2023 study found that 42% of dangerous interactions happen because patients didn’t tell their doctor about their vitamins or herbal remedies. Always disclose everything - and double-check yourself.
What if I get a red alert but my doctor says it’s fine?
Trust your doctor - but ask why. Sometimes, the interaction is managed with monitoring, dose changes, or timing (like taking one med in the morning and the other at night). Ask your doctor: “What are we watching for?” and “What should I do if I feel worse?” Don’t assume silence means safety.
Are herbal supplements really risky with prescription drugs?
Yes - and often more than people realize. St. John’s Wort can make birth control, antidepressants, and blood thinners useless. Garlic and ginkgo can thin your blood dangerously when taken with warfarin. Turmeric can interfere with diabetes meds. Just because something is “natural” doesn’t mean it’s safe with your prescriptions.
How often should I check for interactions?
Check every 30 days, or anytime you start, stop, or change a medication - even if it’s just a new painkiller or sleep aid. Your body’s chemistry changes with age, diet, and health. What was safe last month might not be today.
Can I use these tools for my elderly parents?
Yes - and you should. Seniors are at highest risk for interactions. Use a tablet or phone to help them enter their meds. Print the results and bring them to appointments. Many pharmacies offer free medication reviews for seniors - ask about them.
Next Steps: What to Do Today
If you take more than one medication - even just a daily aspirin and a multivitamin - do this now:- Grab a piece of paper and write down every pill, capsule, and liquid you take - including when and why.
- Go to Drugs.com or WebMD and run your list through their interaction checker.
- If anything shows up as red or yellow, call your pharmacist before doing anything else.
- Set a calendar reminder to check again in 30 days.

Corey Chrisinger
January 17, 2026 AT 03:03Bianca Leonhardt
January 18, 2026 AT 14:49Travis Craw
January 20, 2026 AT 06:36Christina Bilotti
January 22, 2026 AT 05:46Corey Sawchuk
January 24, 2026 AT 05:17Rob Deneke
January 25, 2026 AT 23:37evelyn wellding
January 26, 2026 AT 01:42Chelsea Harton
January 27, 2026 AT 08:09swarnima singh
January 27, 2026 AT 22:09Isabella Reid
January 28, 2026 AT 23:58Jody Fahrenkrug
January 30, 2026 AT 13:06Kasey Summerer
February 1, 2026 AT 08:16Allen Davidson
February 2, 2026 AT 21:33john Mccoskey
February 3, 2026 AT 03:25