Overactive Bladder Drugs: What Works, What to Watch For
When your bladder sends urgent signals you can’t ignore, overactive bladder drugs, medications designed to calm involuntary bladder contractions and reduce frequent urges to urinate. Also known as OAB medications, they’re often the first line of defense for people dealing with sudden leaks, nighttime bathroom trips, or the constant fear of not making it to the toilet in time. This isn’t just about inconvenience—it’s about reclaiming control over daily life, from work meetings to road trips to sleep.
These drugs fall into two main groups: anticholinergics, a class of medications that block nerve signals telling the bladder to contract, and beta-3 agonists, drugs that relax the bladder muscle directly by activating specific receptors. Common anticholinergics include oxybutynin, tolterodine, and solifenacin. Mirabegron is the most widely used beta-3 agonist. Both types reduce urgency and frequency, but they work differently. Anticholinergics often cause dry mouth, constipation, or blurry vision because they affect other parts of the body too. Beta-3 agonists tend to be gentler on the system but can raise blood pressure in some people. Neither fixes the root cause—like nerve damage or pelvic floor weakness—but they do help manage symptoms enough for many to live normally.
Not everyone responds the same. Some people find one drug works perfectly, while others need to try three or four before finding a fit. And sometimes, the side effects are worse than the symptoms. That’s why it’s critical to track what happens when you start—how often you go, how many leaks occur, whether your mouth feels like cotton. Your doctor needs those details to adjust your dose or switch options. Also, these drugs aren’t for everyone. If you have glaucoma, severe constipation, or urinary retention, some of these medications could make things worse. Always review your full health history before starting.
What you won’t find in most drug ads is how often people stop taking them. Many quit within months because of side effects or because they don’t feel better fast enough. But that doesn’t mean the drug didn’t work—it might mean you need a different one, or maybe you need to combine it with pelvic floor exercises, timed voiding, or lifestyle changes like cutting back on caffeine. The best outcomes happen when medication is part of a plan, not the whole plan.
Below, you’ll find real stories and practical guides on how people manage overactive bladder with medication—what worked, what didn’t, and what they wish they’d known before starting. From insurance battles over brand-name prescriptions to switching to generics safely, from spotting dangerous interactions with other meds to understanding why some drugs just don’t click. This isn’t just a list of pills. It’s a collection of real experiences that help you make smarter choices.
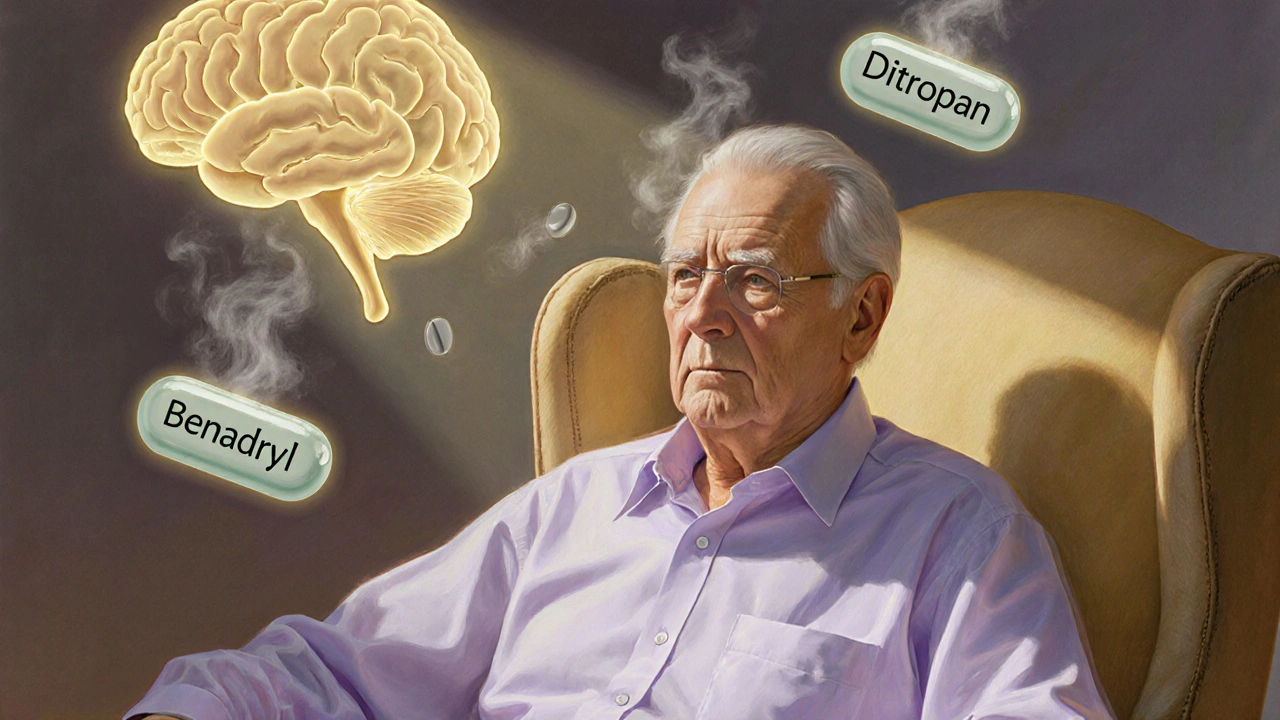
Long-term use of anticholinergic medications like Benadryl, oxybutynin, and amitriptyline is linked to increased dementia risk. Learn which drugs pose the greatest threat, how to check your burden, and safer alternatives.
Read More