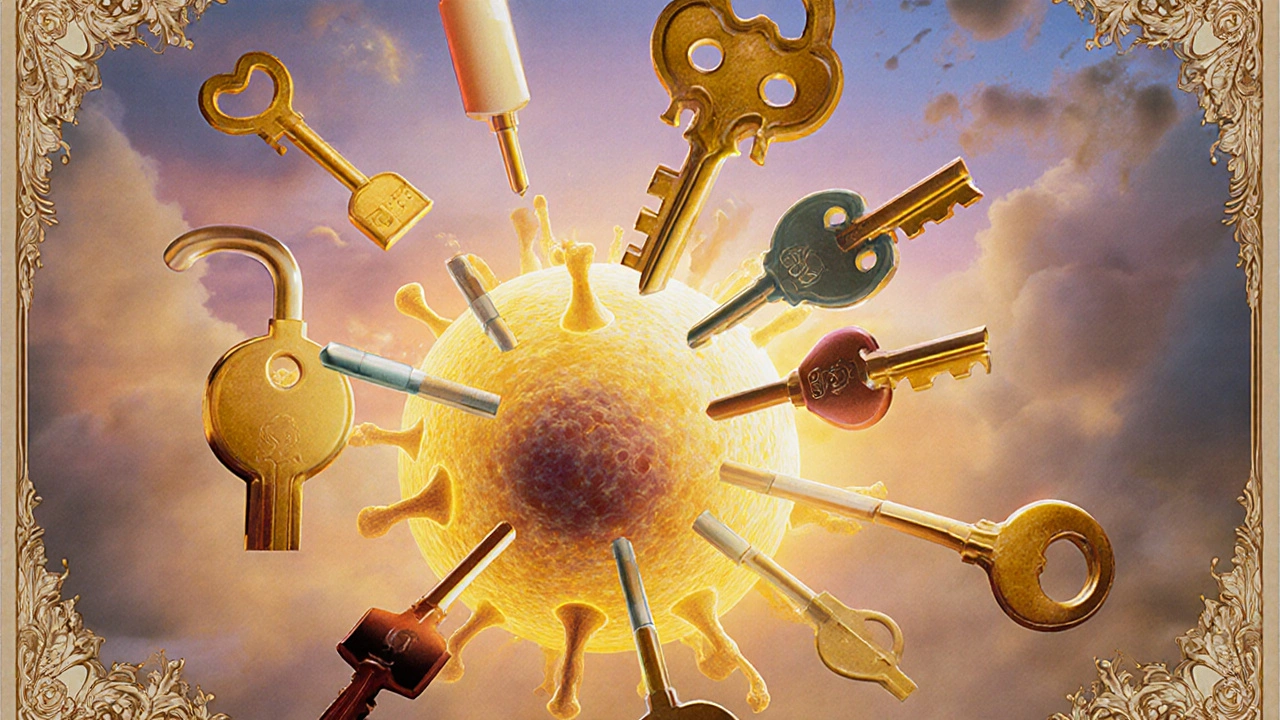
Drug Synergy: How Medications Work Together — Risks and Real-World Examples
When two or more drugs work together in a way that boosts their effect — sometimes far beyond what either could do alone — that’s drug synergy, the combined effect of multiple medications that produces a result greater than the sum of their individual effects. Also known as pharmacological potentiation, it’s not just science fiction — it’s daily practice in hospitals and homes, whether you’re taking antibiotics for an infection or mixing blood pressure meds to get your numbers under control. But synergy isn’t always good. Sometimes it turns safe drugs into hidden dangers.
Take decongestants, over-the-counter nasal sprays and pills like pseudoephedrine that shrink swollen blood vessels. They’re great for a stuffy nose — until you’re also on blood pressure medication, drugs like beta-blockers or ACE inhibitors designed to relax arteries and lower pressure. Together, they can spike your blood pressure to dangerous levels. That’s not synergy you want. Or consider GLP-1 agonists, weight-loss and diabetes drugs like Ozempic and Wegovy, which slow digestion and reduce appetite. When paired with other drugs that affect the pancreas — like certain antibiotics or painkillers — they can increase the risk of pancreatitis. These aren’t edge cases. They’re common mix-ups that land people in the ER.
On the flip side, drug synergy is why some treatments work so well. Cancer patients often get combo chemo because one drug weakens tumor cells, making them easier for the next to kill. Antibiotics like dipyridamole, a blood thinner used to prevent clots, are sometimes paired with aspirin to boost anti-clotting power. Even oral thrush treatments, like nystatin and fluconazole, are chosen based on how they work together against stubborn fungal infections. The key? It’s not about mixing meds randomly. It’s about knowing which combinations are backed by evidence — and which are ticking time bombs.
You won’t find a one-size-fits-all rule for drug synergy. What’s safe for one person can be deadly for another, depending on age, liver function, genetics, or even what you ate for breakfast. That’s why so many of the posts here focus on real-world interactions — from how metformin, a common diabetes drug can trigger lactic acidosis when mixed with certain antibiotics, to why clenbuterol, a fat-burning stimulant often misused for weight loss can throw blood sugar into chaos when combined with insulin or beta-blockers. These aren’t theoretical risks. They’re documented, preventable, and often overlooked.
Below, you’ll find clear, practical guides on exactly which drugs play nice together — and which ones should never share the same bottle. Whether you’re managing diabetes, high blood pressure, chronic pain, or just trying to avoid nasty side effects, you’ll find real examples, step-by-step safety tips, and the kinds of insights you won’t get from a drug label. No fluff. No jargon. Just what you need to stay safe while your meds do their job.
Pharmacodynamic drug interactions happen when drugs change each other's effects at the target site, not by altering their levels in the body. These interactions can be deadly-or lifesaving-and affect millions taking multiple medications.
Read More