Cardiac Inflammation: What It Is and Why It Matters
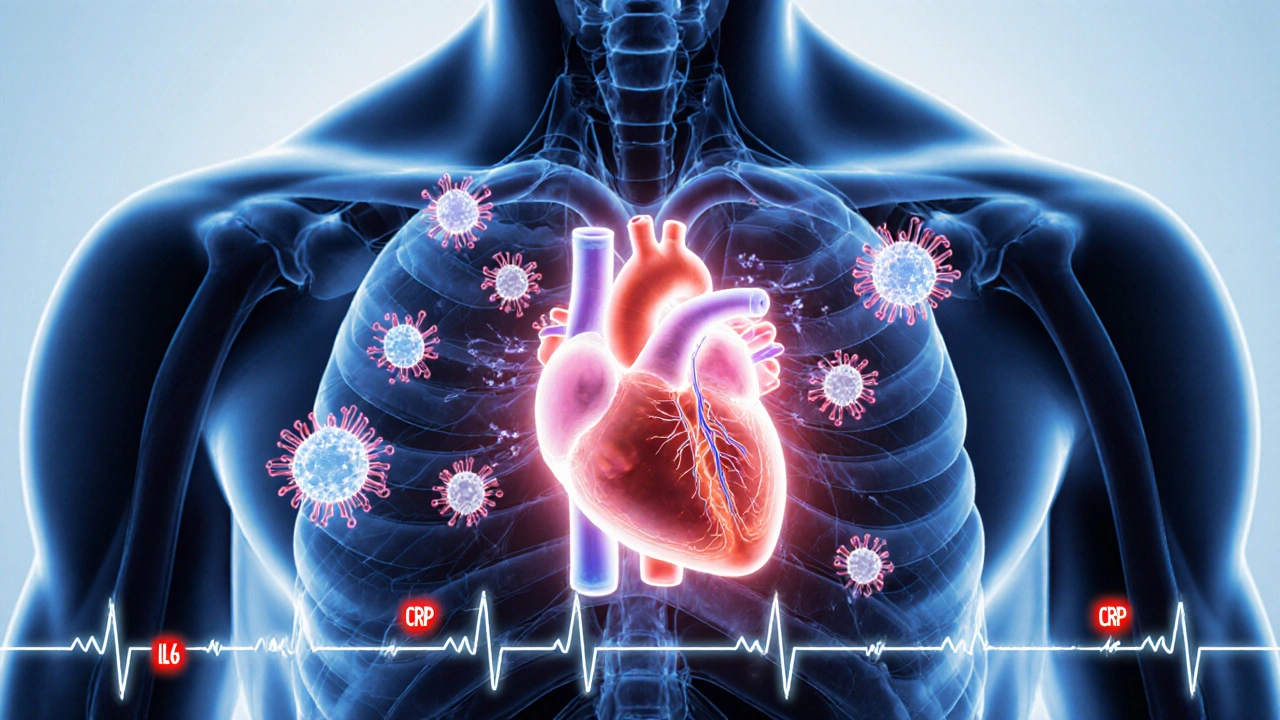
When dealing with cardiac inflammation, the swelling of heart tissue that can disrupt normal rhythm and pumping ability. Also known as heart inflammation, it shows up as chest pain, fatigue, or sudden shortness of breath. Cardiac inflammation isn’t a single disease; it’s an umbrella term that includes several specific conditions. For example, myocarditis, inflammation of the heart muscle often triggered by viral infections and pericarditis, inflammation of the sac surrounding the heart that can cause sharp chest pain are two common forms. An autoimmune response, the body’s mistaken attack on its own tissues can also drive cardiac inflammation, especially in people with systemic lupus or rheumatoid arthritis. This umbrella concept encompasses myocarditis, pericarditis, and even endocarditis, creating a network of related heart disorders.
Key Aspects of Cardiac Inflammation
The causes of cardiac inflammation are diverse. Viral infections such as COVID‑19, influenza or Coxsackie B are top culprits; they influence the heart’s immune environment and can spark myocarditis. Bacterial agents like Staphylococcus can lead to infective endocarditis, while chronic inflammatory diseases trigger an autoimmune response that targets heart tissue. Lifestyle factors—intense endurance training, substance abuse, or exposure to certain toxins—also raise the risk. Early detection requires a mix of tools: an electrocardiogram (ECG) flags rhythm changes, blood tests reveal elevated troponin or C‑reactive protein, and cardiac MRI visualizes tissue swelling. Understanding these diagnostic steps is crucial because untreated inflammation can progress to heart failure or dangerous arrhythmias.
Treatment strategies focus on stopping the inflammation and protecting heart function. For viral‑linked myocarditis, doctors often prescribe anti‑inflammatory drugs like NSAIDs or corticosteroids, sometimes adding colchicine for pericarditis relief. When an autoimmune condition is involved, immunosuppressive therapy (e.g., azathioprine) becomes part of the plan. Lifestyle tweaks—reducing intense workouts, quitting smoking, and managing stress—support recovery. Monitoring is ongoing; repeat imaging ensures the swelling subsides and the heart’s ejection fraction improves. This blend of medication, lifestyle, and follow‑up creates a roadmap that requires coordination between cardiologists, rheumatologists, and primary care providers.
Below you’ll find a curated set of articles that dive deeper into each sub‑topic. Whether you’re looking for a practical guide on diagnosing myocarditis, comparing treatment options for pericarditis, or learning how autoimmune diseases can affect the heart, the collection offers clear, actionable information you can trust.
Explore how irregular heart rhythms affect the immune system, the underlying mechanisms, clinical evidence, and practical steps to protect both heart and immunity.
Read More