Brand-Name Drug Approval: How New Medications Get Approved and What It Means for You
When a company develops a new brand-name drug, a newly invented medication protected by patent and sold under a specific brand name. Also known as innovator drug, it goes through a strict review before reaching pharmacy shelves. This process isn’t just paperwork—it’s a multi-year journey that decides whether a drug is safe, effective, and worth prescribing. The FDA, the U.S. agency responsible for regulating food, drugs, and medical devices doesn’t approve drugs lightly. They look at clinical trial data, manufacturing quality, side effects, and how the drug behaves in the body. If it passes, the drug gets the green light—but only after years of testing and hundreds of millions in investment.
Brand-name drug approval isn’t the end of the story. It’s the starting line for something bigger: drug exclusivity, a period when no generic version can be sold, even after the patent expires. This is where the Hatch-Waxman Act comes in—it balances innovation with access. The FDA gives the original maker up to five years of exclusivity on top of the patent, so they can recoup costs. But once that clock runs out, generic manufacturers can submit an ANDA, an Abbreviated New Drug Application used to prove a generic version is the same as the brand-name drug. That’s when prices drop, and your wallet breathes easier. You might not realize it, but every time you pick up a cheaper generic, you’re seeing the result of this system in action.
What does this mean for you? If you’re on a brand-name drug today, you’re likely paying more because no generic is available yet. But if you’ve switched from a brand to a generic, you’ve benefited from the approval process working as intended. The same rules that keep unsafe drugs off the market also make sure generics are just as effective. That’s why the FDA requires bioequivalence testing—proving the generic delivers the same amount of active ingredient at the same speed as the original. It’s not a copy. It’s a match.
Some brand-name drugs never face generic competition because of legal tricks—patent extensions, new formulations, or lawsuits that delay generics. That’s why you’ll see articles here about effective patent life and why a 20-year patent doesn’t mean 20 years of monopoly. The real window for exclusivity is often much shorter, and knowing that helps you plan ahead. Whether you’re managing a chronic condition, trying to save on prescriptions, or just curious why some drugs cost so much, understanding brand-name drug approval gives you power. You’ll know when a cheaper option is coming, why your doctor might push for a generic, and when it’s worth asking for a switch.
Below, you’ll find real stories and deep dives into how this system affects your health—from how long it takes for a drug to get approved, to why some medications have hidden risks, to how generic competition drives prices down. These aren’t theoretical discussions. They’re based on real cases, real data, and real choices people make every day. Whether you’re on a brand-name drug now or waiting for a generic to arrive, this collection gives you the facts you need to make smarter decisions.
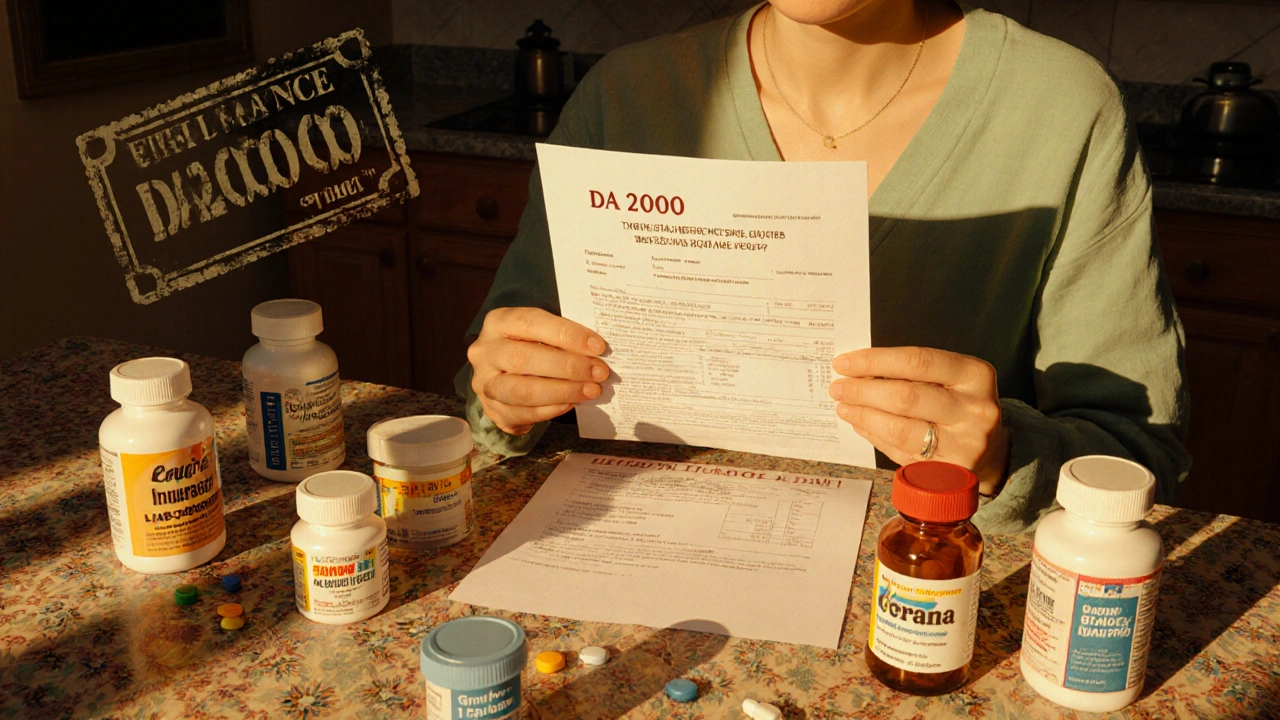
When a generic medication fails to work for you, insurance denials can be frustrating - but not unbeatable. Learn how to fight back with medical evidence, step-by-step appeals, and proven strategies that work.
Read More