Gonorrhea Recovery & ED Timeline Estimator
Estimate your recovery timeline for gonorrhea infection and potential erectile dysfunction based on your treatment adherence and symptoms. This tool helps you understand what to expect during recovery.
When a man hears the words gonorrhea erectile dysfunction, he probably wonders how a bacterial infection could affect his performance in the bedroom. The short answer: untreated gonorrhea can damage the tissues and hormones that control erection, and the anxiety around the infection can make the problem worse. This guide walks you through what gonorrhea is, how it can lead to erectile dysfunction (ED), what symptoms to watch for, and how to get back on track.
Key Takeaways
- Gonorrhea is caused by the bacterium Neisseria gonorrhoeae and can infect the urethra, prostate, and rectum.
- Both physical damage (e.g., inflammation, scarring) and psychological stress from an STD can trigger erectile dysfunction.
- Early detection and proper antibiotic treatment reverse most sexual‑function issues.
- Untreated gonorrhea may lead to chronic prostatitis, which is a common hidden cause of ED.
- Regular STI screening and open communication with partners are the best prevention tools.
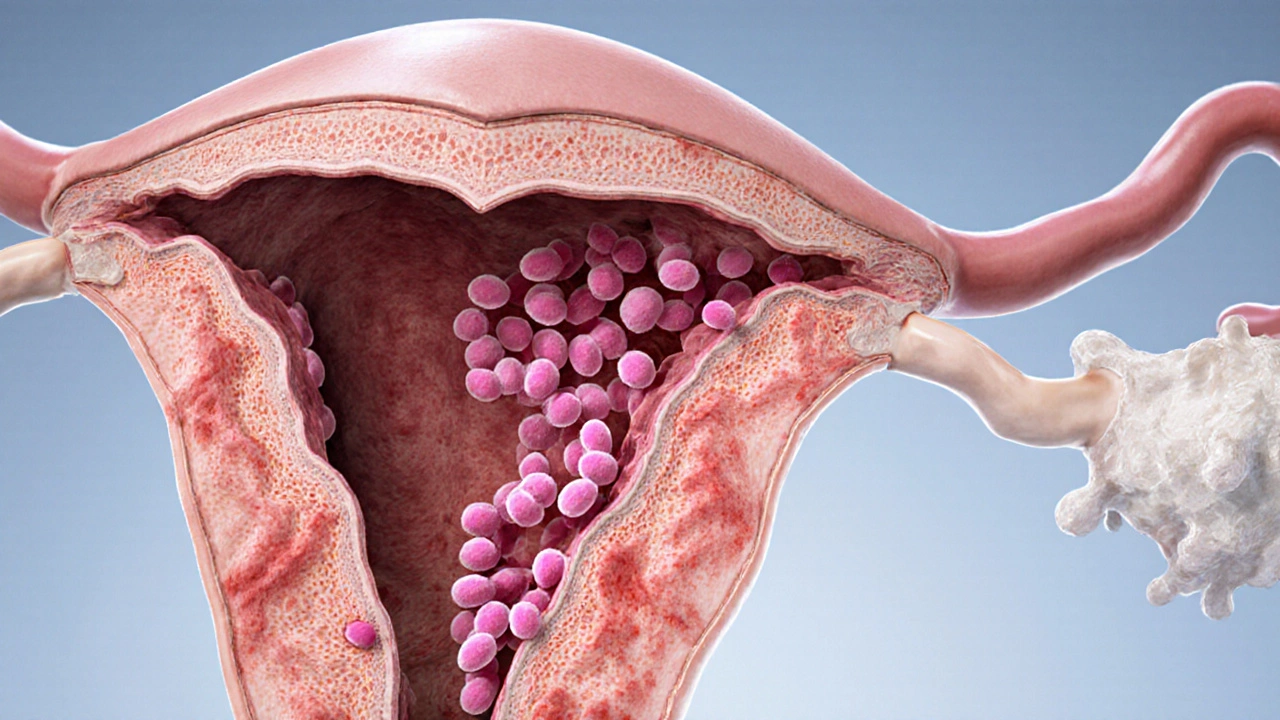
What Is Gonorrhea?
Gonorrhea is a sexually transmitted infection (STI) caused by the Gram‑negative diplococcus Neisseria gonorrhoeae. The bacteria thrive in warm, moist mucous membranes, making the urethra, cervix, rectum, throat, and eyes prime sites for infection.
According to the World Health Organization (WHO), more than 82 million new cases were reported worldwide in 2023, a 10% rise from 2020. Antibiotic resistance is a growing concern, with the CDC flagging azithromycin‑resistant strains as a public health emergency.
Understanding Erectile Dysfunction
Erectile Dysfunction, often shortened to ED, is the consistent inability to achieve or maintain an erection sufficient for sexual activity. It is not a single disease but a symptom that can stem from vascular, hormonal, neurological, or psychological factors.
Key physiological players include:
- Penile blood flow - governed by nitric oxide (NO) release and smooth‑muscle relaxation.
- Testosterone - the primary male hormone that regulates libido and endothelial health.
- Nerve signaling - particularly the pudendal nerve that triggers erection reflexes.
When any of these systems are disrupted, the erection process breaks down.
How Gonorrhea Can Lead to ED
There are three main pathways linking gonorrhea to erectile dysfunction:
- Inflammation and scarring: Untreated gonorrhea often spreads to the prostate (prostatitis) or the urethra, causing chronic inflammation. Over time, scar tissue can narrow the urethra and affect the blood vessels that supply the penis.
- Hormonal imbalance: Persistent infection triggers the body’s stress response, elevating cortisol. High cortisol suppresses testosterone production, leading to reduced libido and weaker erections.
- Psychological impact: The stigma and anxiety of having an STI can cause performance anxiety, a well‑documented cause of situational ED.
Studies from the British Journal of Urology International reported that men with a history of untreated gonorrhea had a 2.3‑fold higher odds of reporting ED three years later, even after adjusting for age, smoking, and diabetes.
Spotting the Symptoms Early
Gonorrhea often presents with mild or no symptoms, which is why routine testing is crucial. When symptoms do appear, they might include:
- Burning sensation during urination
- Pus‑like discharge from the penis
- Painful or swollen testicles
- Rectal pain or discharge (if anal intercourse occurred)
- Sore throat (from oral sex)
ED may manifest as:
- Difficulty achieving an erection
- Reduced rigidity that disappears quickly
- Loss of spontaneous erections (e.g., during sleep)
If you notice any of these signs together, seek medical care promptly.
Diagnosis: What Your Doctor Will Do
Testing for gonorrhea is straightforward:
- Urine NAAT (nucleic acid amplification test) - the gold standard for detecting bacterial DNA.
- Urethral swab - collected by a clinician if the urine test is inconclusive.
- Rectal or pharyngeal swab - recommended for men who report receptive anal or oral sex.
For erectile dysfunction, the clinician may:
- Take a detailed sexual‑health history.
- Measure morning testosterone levels.
- Perform a penile Doppler ultrasound to assess blood flow.
- Screen for cardiovascular risk factors that often coexist with ED.

Treatment Options and Recovery Timeline
Because gonorrhea is bacterial, antibiotics are the cure. Current CDC guidelines (2024 update) recommend a dual‑therapy regimen to combat resistance:
| Drug | Dosage | Purpose |
|---|---|---|
| Ceftriaxone | 500mg IM single dose | Primary gonorrhea kill |
| Doxycycline | 100mg PO twice daily for 7days | Cover possible chlamydia co‑infection |
Most men see symptom relief within 48-72hours. However, if inflammation has already damaged blood vessels, additional steps are needed to address ED:
- PDE5 inhibitors: Medications like sildenafil or tadalafil can temporarily improve blood flow while tissues heal.
- Pelvic floor physiotherapy: Strengthening the muscles around the penis aids erectile rigidity.
- Hormone therapy: If testosterone levels are low, a short course of testosterone replacement can restore libido.
- Psychological counseling: Cognitive‑behavioural therapy helps break the anxiety‑ED cycle.
Full recovery of erectile function typically occurs within 3-6months after the infection clears, assuming no permanent scarring.
Preventing Future Infections and Protecting Sexual Wellness
Prevention is a blend of behaviour and medical vigilance:
- Use condoms consistently and correctly. They reduce gonorrhea transmission by ~70%.
- Get tested at least annually if you have multiple partners, or sooner after any unprotected encounter.
- Inform partners about your STI status - partner treatment prevents reinfection.
- Maintain a healthy lifestyle: regular exercise, balanced diet, and limiting alcohol improve both immune function and erectile health.
Vaccines for gonorrhea are still in development, with a promising phase‑III trial expected to report results in 2026. Until then, vigilance remains the best shield.
Frequently Asked Questions
Can a single episode of gonorrhea cause permanent erectile dysfunction?
Most men recover fully once the infection is treated promptly. Permanent ED is rare and usually linked to chronic prostatitis or severe scarring that develops after repeated or untreated infections.
Do I need to take antibiotics for my partner too?
Yes. The CDC recommends simultaneous treatment of all sexual partners within 60days of diagnosis to prevent reinfection and further spread.
Is it safe to use PDE5 inhibitors while taking antibiotics?
Generally, PDE5 inhibitors do not interact with the antibiotics used for gonorrhea. However, discuss any heart conditions or other meds with your doctor, as some combinations can affect blood pressure.
How long should I wait before trying sex again?
Abstain from intercourse until you have completed the full antibiotic course and a follow‑up test (usually 1week later) confirms the infection is cleared. This also gives the inflamed tissues time to heal.
What lifestyle changes help reduce the risk of ED after an STI?
Quit smoking, limit excessive alcohol, maintain a healthy weight, exercise regularly, and manage stress. These habits improve vascular health and hormone balance, both crucial for erections.
Next Steps If You Suspect Gonorrhea or ED
- Schedule a visit with your primary care provider or a sexual‑health clinic.
- Ask for a NAAT test for gonorrhea (and chlamydia) even if you feel fine.
- Discuss any erection concerns openly - the doctor can order hormone panels and vascular studies.
- Follow the prescribed antibiotic regimen exactly; do not self‑medicate.
- If ED persists after treatment, request a referral to a urologist or a men's health specialist.
Taking action early not only clears the infection but also safeguards your confidence and intimacy.
Ian McKay
October 12, 2025 AT 05:32While the article is generally accurate, the phrase “tissues and hormones that control erection” could be tightened to “tissues and hormones governing erection.” Also, “the infection clears” reads better as “the infection is cleared.” Minor tweaks improve clarity.
Deborah Messick
October 12, 2025 AT 13:52It must be emphasized, dear readers, that the presented correlation between gonorrhea and erectile dysfunction, though documented, is not universally deterministic. To ascribe a causal relationship without acknowledging the myriad vascular and psychogenic factors would be an oversimplification bordering on sensationalism. One ought to consider the broader epidemiological landscape before arriving at any hasty conclusions.
Jolanda Julyan
October 12, 2025 AT 22:12First, thank you for putting together such a thorough guide; it covers the essential points that many readers need to understand. The link between untreated gonorrhea and erectile dysfunction is indeed a serious matter, and the article does a good job of outlining the physiological pathways. Inflammation in the prostate can scar tissue, which in turn hampers blood flow to the penis, a fact that cannot be ignored. Hormonal imbalance, particularly suppressed testosterone due to chronic stress, adds another layer of complication that many men overlook. Psychological stress stemming from the stigma of an STI often leads to performance anxiety, creating a feedback loop that worsens erectile function. The article rightly highlights that early detection and treatment can reverse most of these issues if managed properly. However, it could go further by stressing the importance of routine screening even for asymptomatic individuals. Many men mistakenly believe that lack of symptoms means they are in the clear, which is a dangerous misconception. The recommendation of using condoms consistently is a cornerstone of prevention and should be reiterated throughout the piece. Additionally, mentioning the rising antibiotic resistance provides a timely reminder that treatment protocols are evolving. Readers would benefit from a brief overview of alternative therapies should first‑line antibiotics fail. The suggestion to incorporate pelvic floor physiotherapy is a valuable addition, as strengthening these muscles can improve erectile rigidity. Hormone therapy is appropriately presented as a conditional option, pending lab results, which prevents unnecessary self‑medication. The article’s balanced approach to both medical and lifestyle interventions respects the complexity of sexual health. Finally, the call to open communication with partners cannot be overstated; it fosters trust and encourages mutual responsibility. Overall, the guide is comprehensive, but integrating these extra points would make it an even more robust resource for men navigating gonorrhea and its potential impact on erectile function.
Kevin Huston
October 13, 2025 AT 06:32Look, if you think the U.S. healthcare system is magically fixing this, you’re in for a rude awakening – antibiotics alone won’t save you from a messed‑up love life if you keep ignoring basic safe‑sex practices.
Amanda Hamlet
October 13, 2025 AT 14:52Honestly, most people just dont read the fine print about how smoking worsens the recovery timeline. You can keep ignoring it, but the facts are clear – smoking + gonorrhea = longer ED. Just saying.
Nolan Jones
October 13, 2025 AT 23:12Good eye on the phrasing, Ian. Adding a note about the importance of follow‑up testing after treatment can also help readers avoid lingering issues.
Jada Singleton
October 14, 2025 AT 07:32The moral high ground you take, Deborah, feels a bit preachy, but you do raise a valid point about not jumping to conclusions.
Emily Rossiter
October 14, 2025 AT 15:52Jolanda, you covered the bases nicely. I’d add that keeping a symptom diary can help doctors tailor the best treatment plan.
Renee van Baar
October 15, 2025 AT 00:12Kevin, your point hits home – safe sex isn’t just a buzzword, it’s a real shield against both infection and the downstream complications like ED.
Mithun Paul
October 15, 2025 AT 08:32While the colloquial expression employed by the preceding commentator captures the sentiment, a more rigorous articulation would underscore that adherence to prophylactic measures substantively mitigates the incidence of sexually transmitted infections and their sequelae.
Sandy Martin
October 15, 2025 AT 16:52I appreciate how the guide balances medical facts with practical advice, making it accessible for men who might feel embarrassed about the topic.
Steve Smilie
October 16, 2025 AT 01:12Indeed, the exposition transcends mere didacticism, venturing into a nuanced discourse that marries clinical precision with lyrical eloquence.
Josie McManus
October 16, 2025 AT 09:32Reading this made me think about how many friends I've known who suffered in silence; sharing this info could actually save someone from months of unnecessary distress.
Heather Kennedy
October 16, 2025 AT 17:52The psychosocial dimension you highlight aligns with current literature on stigma‑related sexual dysfunction, where cognitive‑behavioral frameworks are often employed to dismantle maladaptive beliefs.
Janice Rodrigiez
October 17, 2025 AT 02:12Great point – tackling the mental side is key, and tools like CBT can really shift the narrative for men dealing with post‑STI anxiety.
Roger Cardoso
October 17, 2025 AT 10:32One might wonder whether the pharmaceutical industry’s push for broad‑spectrum antibiotics is subtly masking a deeper issue of overprescription, potentially accelerating resistance trends.
barry conpoes
October 17, 2025 AT 18:52While conspiracy theories are tempting, the data clearly shows that antibiotic stewardship programs have reduced resistance when properly implemented, underscoring the need for evidence‑based policies.
Kristen Holcomb
October 18, 2025 AT 03:12Do you think we could see a shift toward more personalized antimicrobial regimens as genomic sequencing becomes cheaper?
justin davis
October 18, 2025 AT 11:32Wow, groundbreaking stuff, really.