Rare Side Effect Detection Calculator
Based on the article: Clinical trials often miss rare side effects. For example, a Phase 3 trial with 381 patients might not detect a side effect occurring in 1 out of 1,000 patients. This calculator shows how trial size affects detection probability.
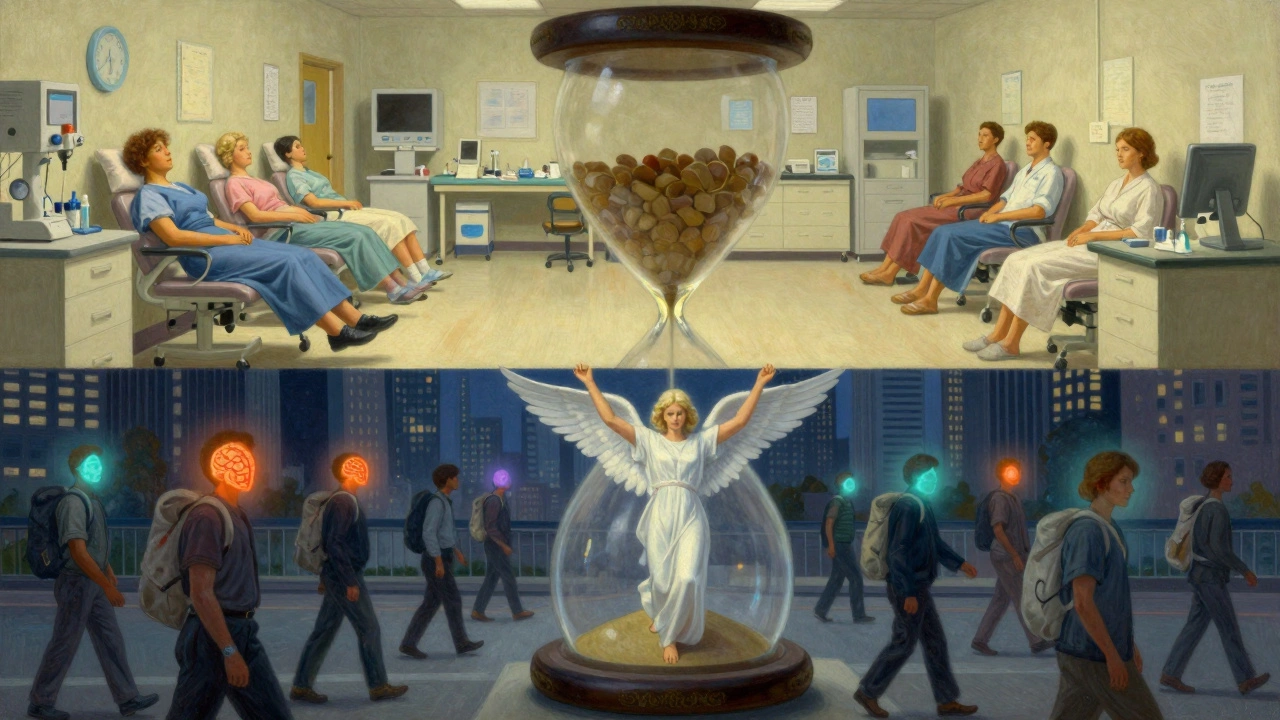
When you take a new medication, you might read the label and see a long list of possible side effects. But here’s the thing: many of those side effects were never seen in the clinical trials that got the drug approved. And some side effects you’ve heard about from other patients? They might not show up in any official report at all. Why? Because clinical trial data and real-world side effect data aren’t the same thing. They don’t even try to measure the same things.
What Clinical Trials Actually Measure
Clinical trials are designed to answer one question: does this drug work under ideal conditions? To get that answer, researchers pick people who fit very specific criteria. They’re usually healthy enough to handle the study, not taking other drugs that could interfere, and closely monitored every week or two. These trials use strict rules to track side effects - like the Common Terminology Criteria for Adverse Events (CTCAE), which has 790 exact terms for everything from mild nausea to death.That sounds thorough, right? But here’s the catch: the average Phase 3 trial for a cancer drug includes just 381 people. That’s not enough to spot side effects that happen in 1 out of 1,000 patients. If something rare occurs, it’s likely to be missed. And if a side effect only shows up after six months? Most trials end at three or four. That’s why drugs like rosiglitazone got approved in 1999 - and then years later, real-world data showed users had a 43% higher risk of heart attacks.
Clinical trials are great at proving cause and effect. If a group taking the drug gets more headaches than the placebo group, and the trial was randomized and double-blind, you can be pretty sure the drug caused it. That’s why regulators like the FDA still require them before approving any new medicine.
What Real-World Data Shows That Trials Miss
Real-world data comes from everywhere: doctor’s notes, pharmacy records, insurance claims, patient apps, and reports sent to the FDA’s Adverse Event Reporting System (FAERS). In 2022 alone, FAERS got over 2.1 million reports - up from 1.4 million in 2018. These aren’t controlled studies. They’re messy. People take multiple drugs. They have other health problems. They forget to tell their doctor about a new rash. But that’s exactly why this data matters.Real-world data caught the link between pioglitazone and heart failure after 10 years of use. It flagged dangerous side effects from fluoroquinolone antibiotics - like tendon ruptures and nerve damage - after analyzing 1.2 million patient records. It even spotted early warnings about ivermectin misuse on Twitter 47 days before official reports came in.
And it’s not just rare events. A 2022 survey by the National Patient Advocate Foundation found that 63% of patients experienced side effects not listed on their drug’s FDA-approved label. Over 40% of those were moderate to severe - affecting sleep, work, or daily life. Pharmacists on Reddit say 78% of them see mismatches between trial reports and what patients actually experience, especially with newer drugs like GLP-1 agonists for weight loss. Patients report fatigue, nausea, or brain fog that trials didn’t capture because they only asked about symptoms during office visits - not at home, late at night, or after a long workday.

Why Real-World Data Can Be Misleading
Just because real-world data finds a pattern doesn’t mean it’s real. In 2018, a big study claimed anticholinergic drugs (used for allergies, depression, and overactive bladder) increased dementia risk. But later analysis showed those patients were already sicker - they had more urinary issues, more depression, more sleep problems. The drugs weren’t causing dementia; the underlying conditions were. Real-world data can’t control for that. It sees correlation, not causation.And then there’s the reporting problem. Only 2-5% of actual side effects make it into FAERS, according to the Agency for Healthcare Research and Quality. Why? Doctors are busy. Reporting takes an average of 22 minutes per case. A 2021 AMA survey found only 12% of physicians report adverse events consistently. Patients don’t report either - unless they’re using tools like the MyTherapy app, which found 27% more fatigue reports from immunotherapy patients than clinical trials did. Why? Because patients track symptoms daily, not just when they see their doctor.
How the FDA Uses Both Types of Data
The FDA doesn’t treat these as rivals. They’re partners. Clinical trials tell them: “This drug works, and here are the most common risks.” Real-world data tells them: “But here’s what happens when millions of people take it - including seniors, pregnant women, and those with five other conditions.”In 2022, 67% of new drug approvals included real-world evidence in post-marketing requirements. That’s up from 29% in 2017. The FDA’s Sentinel Initiative now monitors 300 million patient records in near real-time. It uses 17 different statistical methods to spot safety signals - like a sudden spike in liver damage reports after a new drug hits the market. But even Sentinel needs months to confirm a signal. That’s why the agency now requires all new drug applications to include a plan for collecting real-world data after launch.
Still, the rules aren’t the same everywhere. The European Union still requires clinical trials to confirm new safety signals. The FDA is more flexible - allowing real-world data to support label changes, like adding warnings about long-term risks. But it won’t approve a drug based on real-world data alone.
What This Means for Patients and Doctors
If you’re a patient, don’t assume the drug label tells you everything. If you feel something unusual - especially if it’s not on the list - talk to your doctor. Write it down. Track it. Use an app. You’re not just a number in a trial; you’re part of the real-world data pool.If you’re a doctor, learn to read both types of data. A 2023 study found only 38% of physicians could correctly interpret real-world evidence without training. You need to know when a side effect reported by a patient is a fluke - or a warning sign. And you need to know that if 10 patients tell you about the same weird symptom, it’s worth investigating - even if the trial said it was rare.
The Future: Blending Both Worlds
The biggest shift happening now is hybrid trials. Companies like Pfizer and Novartis are starting to collect real-world data during late-stage clinical trials. Patients use wearables to track sleep, heart rate, and mood. They report symptoms via apps. This gives researchers both the control of a trial and the breadth of real-world use - all at once.AI is helping too. Google Health’s 2023 study analyzed 216 million clinical notes and found 23% more drug-side effect links than traditional methods. Apple’s Heart Study, with over 400,000 participants, showed how smartphones can capture data at trial scale - without needing a clinic visit.
But experts agree: real-world data won’t replace clinical trials. It will complement them. Trials give us the first safety snapshot. Real-world data gives us the full-length movie.
The bottom line? Side effects aren’t just in the brochure. They’re in your experience, your doctor’s notes, your pharmacy records, and the millions of data points collected every day. The most complete picture comes from listening to both - the science of the trial and the truth of everyday life.

Nathan Fatal
December 11, 2025 AT 22:34Clinical trials are a necessary evil-they give us control, but they’re like studying a fish in a fishbowl and pretending it represents the whole ocean. Real-world data is the messy, noisy ocean. It’s where the real story lives. I’ve seen patients on GLP-1s report brain fog so bad they couldn’t work, but the trials only asked about nausea and diarrhea. That’s not oversight-it’s design. We’re not measuring what matters to people, just what’s easy to count.
Donna Anderson
December 12, 2025 AT 05:38my dr just told me to ‘tough it out’ when i started getting dizzy on my new med… turns out 3 other ppl in the waiting room had the same thing. no one’s tracking this stuff. why do we still act like trials = truth?
Laura Weemering
December 12, 2025 AT 07:44Let’s be honest: the FDA’s entire model is built on a 20th-century assumption-that human biology is linear, predictable, and controllable. But we’re not lab rats. We’re complex, comorbid, polypharmaceutical beings. The real-world data isn’t ‘messy’-it’s authentic. The trials? They’re sanitized fiction. And yet, we still treat them like scripture. It’s not ignorance-it’s institutional arrogance.
Reshma Sinha
December 14, 2025 AT 05:48As a pharmacist in Mumbai, I see this daily. Patients come in with side effects no label mentions-especially with newer drugs. One guy on semaglutide had severe insomnia but didn’t report it because he thought it was ‘just stress.’ We need better systems to capture this-not just FAERS, but community-based reporting. Real people, real lives.
Adam Everitt
December 14, 2025 AT 20:51the thing no one talks about is that trials are designed to fail as little as possible… not to reveal truth. it’s marketing with a lab coat. and the FDA? they’re just the gatekeeper for pharma’s PR machine. real-world data exposes the lie. but who benefits from that? not patients.
wendy b
December 16, 2025 AT 05:26While I appreciate the sentiment, one must acknowledge that real-world data lacks methodological rigor. Without randomization, blinding, and control groups, correlation is not causation. The FDA’s cautious stance is not bureaucratic inertia-it’s scientific integrity.
Ashley Skipp
December 16, 2025 AT 23:30glp1s are just a fancy diet pill and everyone’s acting like it’s medicine stop pretending your brain fog is a medical mystery its just your body saying you’re eating too little
Stacy Foster
December 18, 2025 AT 15:24They’re hiding the side effects on purpose. The same people who approved Vioxx and thalidomide are still running the FDA. Real-world data is the only thing keeping us alive. Don’t trust the system. Track your symptoms. Share them. They don’t want you to know how many people they’re killing quietly.
Robert Webb
December 19, 2025 AT 16:53I’ve been a primary care doc for 22 years, and I can tell you this: the gap between clinical trial data and real-world experience isn’t a bug-it’s a feature of how medicine is structured. Trials are for approval. Real-world data is for adaptation. The problem is we don’t train doctors to read either properly. We teach them to memorize labels, not interpret patterns. If 10 patients tell you they’re having weird fatigue on a new drug, that’s not anecdotal-it’s a signal. And if your EMR doesn’t let you tag it, that’s a system failure, not a patient failure.
nikki yamashita
December 20, 2025 AT 02:39YES. my mom had a rash for 3 weeks after starting her new med. dr said ‘not in trials so probably not related.’ she went to urgent care and they said ‘this is a known reaction we just haven’t updated the label yet.’ we need apps that let patients report in real time. not just after they’re hospitalized.
Rob Purvis
December 21, 2025 AT 03:02It’s fascinating how we’ve built a medical system that prioritizes regulatory efficiency over patient lived experience. The FDA’s Sentinel Initiative is a step forward, but it’s still reactive. What if we had real-time, patient-driven dashboards-like a public health dashboard for drug side effects, updated daily? Imagine if you could see, in your region, how many people are reporting brain fog on Ozempic. That’s not conspiracy. That’s transparency.
Lawrence Armstrong
December 22, 2025 AT 01:04My wife’s on a GLP-1. She’s had night sweats, muscle cramps, and zero appetite for 4 months. The label says ‘mild nausea.’ I tracked her symptoms in MyTherapy. After 6 weeks, it flagged a pattern. We showed it to her doctor. They added it to the local safety report. Small win. But why should it be on us to do the work of the FDA?
😔Levi Cooper
December 22, 2025 AT 03:18Look, if you’re not an American citizen, you don’t get to complain about FDA rules. We have the best drug approval system in the world. If you can’t handle a little fatigue or brain fog, maybe you shouldn’t be on medication. Other countries are still using 1970s tech. We’re leading the future. Stop whining.