When a child isn’t growing like they should-staying small for their age, losing weight, or seeming tired all the time-it’s easy to blame picky eating or slow metabolism. But sometimes, the real issue is hidden in plain sight: celiac disease. It’s not just a food allergy. It’s an autoimmune condition that quietly damages the gut, steals nutrients, and stunts growth. And if it’s missed, the damage can last a lifetime.
Why Growth Problems Are a Red Flag
In kids, celiac disease doesn’t always show up with stomach pain or diarrhea. Many children have no obvious digestive symptoms at all. Instead, the first sign is often slow growth. A child who’s been on the 50th percentile for height since infancy suddenly drops to the 10th. Or they’re tall for their age but don’t gain weight. These aren’t just quirks-they’re warning signs. Studies show that up to 40% of children diagnosed with celiac disease are first identified because they’re shorter than expected. Their bodies aren’t absorbing iron, calcium, vitamin D, or protein. Without those, bones don’t strengthen, muscles don’t build, and growth plates don’t mature properly. The gut lining gets flattened. Imagine a sponge that’s been crushed flat-same idea. The surface area for absorbing food drops by 60 to 90%. No matter how much they eat, they’re starving at a cellular level. The good news? Growth almost always bounces back. But timing matters. Kids diagnosed before age 5 have a 98% chance of reaching their full adult height with a strict gluten-free diet. After age 10, that drops to 85%. The earlier you catch it, the better the outcome.How Doctors Test for Celiac Disease Today
Testing has gotten smarter. Ten years ago, every child with suspected celiac got an endoscopy. Now, many don’t need one. The first step is a simple blood test: tTG-IgA. It looks for antibodies your body makes when gluten damages the gut. If the result is 10 times higher than normal-and the child has HLA-DQ2 or DQ8 genes (which 95% of celiac patients carry)-doctors can diagnose celiac without a biopsy. That’s a big deal. Fewer needles, less stress, faster answers. But here’s the catch: the test only works if the child is still eating gluten. If you’ve already switched to gluten-free before testing, the antibodies drop, and the test looks normal. That’s why doctors won’t test a child who’s been on a gluten-free diet for more than a few weeks. You have to eat gluten for at least 6 weeks before testing, even if it makes them feel worse. If the blood test is borderline, or if the child has IgA deficiency (which happens in 2-3% of celiac cases), a biopsy is still needed. During an endoscopy, a tiny tube goes down the throat to take samples from the small intestine. Under the microscope, doctors look for Marsh 3 lesions-flattened villi, inflamed tissue, the classic fingerprint of celiac disease. Bone age X-rays are another tool. Many kids with undiagnosed celiac have bones that are 1.5 to 2.5 years behind their real age. That delay is actually a good sign-it means they still have time to catch up. Once gluten is gone, their growth plates kick back in.What a Gluten-Free Diet Really Means
Gluten isn’t just bread and pasta. It’s in soy sauce, malt vinegar, processed meats, some vitamins, and even lip balm. The legal limit for “gluten-free” is 20 parts per million (ppm)-less than a grain of salt in a whole loaf of bread. But cross-contamination is everywhere. A kitchen with shared toasters, cutting boards, or fryers can ruin a gluten-free meal. One study found that 40-50% of households with a child with celiac still have gluten hidden in plain sight. A child might be eating perfectly at home, then get sick after school lunch or a birthday party. The diet isn’t about “eating healthy.” It’s about total avoidance. No exceptions. No “just a bite.” Even tiny amounts keep the immune system active, preventing healing. That’s why tTG-IgA levels are checked every 6 to 12 months. If the antibodies stay high, it means gluten is still getting in-maybe from sauces, medications, or even playdough. The good news? Gluten-free options are more common than ever. But they’re expensive. A box of gluten-free pasta costs 156-242% more than regular. Families spend an extra $1,000 to $2,000 a year just on food. That’s why insurance coverage and school accommodations are so important.
How to Know If the Diet Is Working
You can’t just wait for symptoms to disappear. You need to measure progress. In the first 6 months, most kids gain 15-30 grams of weight per day. That’s about 1 to 2 pounds a month. Height catches up slower. It takes 18 to 24 months for growth velocity to normalize. A child who was growing 3 cm a year might jump to 5-7 cm after starting the diet. Iron levels should rise within 3 months. Vitamin D and B12 follow. If they don’t, supplements are needed. Many kids need iron pills, vitamin D drops, or even B12 injections at first. The biggest clue? Bone age catching up. If a child’s bone age was 7 when they were chronologically 9, and it’s now 9.5 after 18 months on the diet, they’re healing. Their body is finally getting what it needs.Why Adherence Falls Apart-And How to Fix It
The hardest part isn’t the food. It’s the loneliness. A 14-year-old might skip school lunch because they’re the only one with a separate tray. A 7-year-old might sneak crackers because everyone else is eating pizza. Adolescents are 25-35% less likely to stick to the diet than younger kids. Peer pressure, identity, rebellion-it all plays a role. Schools need 504 plans. Not just “no bread,” but dedicated prep areas, trained staff, and clear protocols for field trips and parties. One study found 58% of kids with celiac get exposed at school. That’s unacceptable. Support groups help. Families who connect with local celiac chapters see 25-30% better adherence. Talking to other parents who’ve been there-someone who knows which brands are safe, which restaurants won’t cross-contaminate, how to talk to teachers-makes all the difference. And parents need training. One nutritionist told me a family came in after 8 months on the diet, still struggling. They thought “wheat-free” meant gluten-free. They didn’t know barley was in some soups. They didn’t know oats could be contaminated. It took three visits to get them up to speed.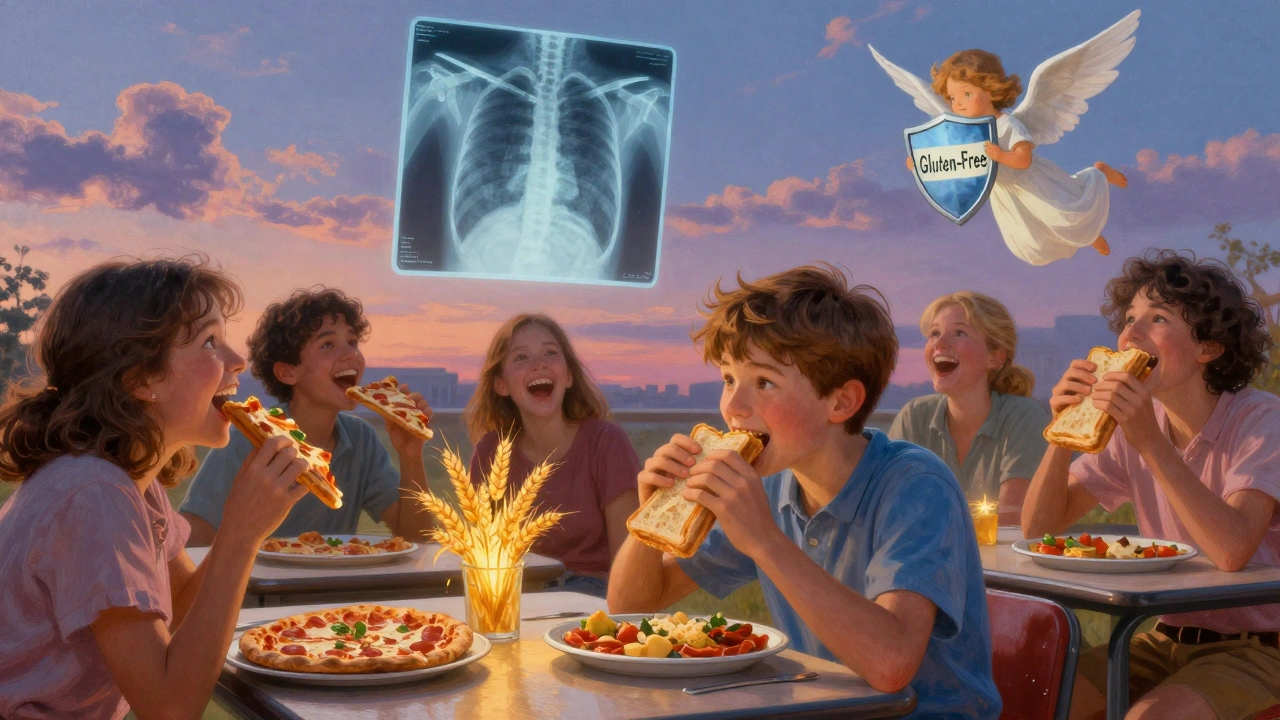
What If Growth Doesn’t Catch Up?
Most kids do. But 5-10% don’t, even with perfect diet adherence. That’s when you dig deeper. Is there another condition? Hypothyroidism? Growth hormone deficiency? Inflammatory bowel disease? These can mimic or worsen celiac symptoms. A child who’s not growing despite strict diet needs a full endocrine workup. The American Academy of Pediatrics says this: if bone age was delayed at diagnosis, the child has a 95% chance of reaching target height. If bone age was normal? Only 65%. That’s why early diagnosis matters. The body’s window for catching up closes with time.What’s Next for Celiac Treatment?
Right now, the only treatment is diet. But research is moving fast. Drugs like larazotide acetate are in Phase 3 trials. They don’t cure celiac, but they help block gluten from leaking into the gut, reducing symptoms after accidental exposure. Think of it like a shield-not a cure, but a safety net. Immunotherapy trials, like Nexvax2, were promising at first but failed in later stages. For now, diet is still king. The future might include pills that break down gluten in the stomach or vaccines that train the immune system not to react. But none of these are ready. Not yet. And they won’t replace the diet.Real Stories, Real Results
One mother in Birmingham told me her son was 3 years old when he was diagnosed. He weighed 25 pounds. He couldn’t run without getting winded. After 3 months on the diet, he gained 5 pounds. At 18 months, he was back on the 50th percentile for height. He’s 10 now. Taller than his older brother. Another family struggled for two years. Their daughter kept getting stomachaches. She was on the diet, but the antibodies stayed high. They finally found out: her favorite yogurt had malt flavoring. One ingredient. One mistake. Once they switched brands, everything changed. There’s hope here. Celiac disease isn’t a life sentence. It’s a switch. Flip it off-gluten-and the body starts healing. The gut repairs. The bones strengthen. The child grows. It’s not easy. But it’s possible. And for every child who gets diagnosed early, it’s a chance to live a full, healthy, normal life.Can a child outgrow celiac disease?
No. Celiac disease is a lifelong autoimmune condition. The body will always react to gluten. There’s no cure, and no amount of time on a gluten-free diet changes the underlying genetics. Even if symptoms disappear, the gut damage can return if gluten is reintroduced. Strict avoidance must continue forever.
What happens if a child accidentally eats gluten?
A single accidental exposure won’t cause permanent damage, but it will trigger inflammation and restart the healing process. Symptoms like stomach pain, fatigue, or diarrhea can appear within hours and last days. More importantly, it keeps tTG-IgA antibodies high, which slows gut repair and growth recovery. That’s why even small amounts matter-like crumbs from a shared toaster or sauce with hidden wheat.
Do all children with celiac disease have digestive symptoms?
No. In fact, many children show no stomach problems at all. Instead, they might have delayed growth, anemia, dental enamel defects, irritability, or chronic headaches. Some are diagnosed only after a sibling or parent tests positive. That’s why screening is recommended for kids with type 1 diabetes, Down syndrome, or a family history of celiac-even if they feel fine.
Is a gluten-free diet healthy for a child without celiac disease?
Not necessarily. Gluten-free processed foods are often lower in fiber, iron, and B vitamins, and higher in sugar and fat. Unless a child has celiac disease, non-celiac gluten sensitivity, or a wheat allergy, there’s no proven benefit to avoiding gluten. In fact, unnecessarily restricting grains can lead to nutritional gaps in growing children. Only follow a gluten-free diet if it’s medically necessary.
How often should a child with celiac disease have follow-up tests?
Blood tests (tTG-IgA) should be done every 6 to 12 months in the first few years after diagnosis to check diet adherence. After that, annual testing is usually enough. Growth should be tracked every 3 to 6 months. Nutrient levels (iron, vitamin D, B12, folate) should be checked at diagnosis and then every 6 to 12 months until they normalize. Bone age X-rays are typically done once at diagnosis to predict catch-up potential.
Can a child with celiac disease eat oats?
Pure, uncontaminated oats are generally safe for most children with celiac disease after the gut has healed. But most oats are processed in facilities that also handle wheat, barley, or rye. Only use oats labeled “gluten-free” and certified by trusted organizations. Introduce them slowly after 6-12 months on the diet, and watch for symptoms. If in doubt, skip them.
What should parents do if their child refuses to follow the diet?
Start with education-not punishment. Help your child understand why the diet matters, using age-appropriate language. Connect them with other kids who have celiac through support groups. Work with the school to create a safe environment. Involve a dietitian who specializes in pediatric celiac. For teens, counseling can help address feelings of isolation or rebellion. The goal is to build long-term self-management, not short-term compliance.

Elizabeth Crutchfield
December 3, 2025 AT 11:49my kid wasnt growing right and we thought it was just picky eating… turns out it was celiac. best thing we ever did was get him tested. no more tired all the time.
Karl Barrett
December 4, 2025 AT 15:39the real kicker is how the immune system keeps firing even with trace gluten. it’s not just about avoiding bread-it’s about the microscopic contamination in soy sauce, vitamins, even lip balm. the gut’s villi are like a forest of microvilli, and gluten turns them into barren plains. it’s a silent war at the cellular level.
Jake Deeds
December 6, 2025 AT 14:50people think gluten-free is just a fad, but if your kid’s growth plates are shutting down because of a protein they don’t even realize they’re consuming… that’s not a trend. that’s medical negligence waiting to happen. and yes, I’ve seen parents blame ‘bad genetics’ for years before testing.
George Graham
December 7, 2025 AT 19:15as a dad of a 7-year-old with celiac, I can tell you the loneliness hits harder than the symptoms. my son used to cry before school lunches because he was the only one with his own container. we found a local support group-changed everything. now he brings his own snacks and even teaches other kids which brands are safe. it’s not just diet, it’s identity.
John Filby
December 9, 2025 AT 11:19so i just found out my niece has it… and i had no idea oats could be contaminated?? 😅 i always thought gluten-free = no wheat. now i’m gonna check every label with a magnifying glass. thanks for the heads up!
Ben Choy
December 10, 2025 AT 07:32my sister’s kid was diagnosed at 4-grew 6 inches in 18 months after going GF. it’s like flipping a switch. but the cost? holy moly. we spent $2k last year just on pasta and bread. insurance needs to step up.
Emmanuel Peter
December 11, 2025 AT 05:02how many of these kids are misdiagnosed as ADHD because they’re tired and irritable? i bet half the kids on Ritalin would be fine if they just stopped eating gluten. this is a systemic failure in pediatrics.
Ollie Newland
December 12, 2025 AT 23:24the tTG-IgA test being 10x above normal as a diagnostic cutoff? that’s gold. no biopsy needed? that’s huge. less trauma for kids, faster answers. the medical system finally got something right.
Carolyn Ford
December 13, 2025 AT 17:10Why are we still letting schools get away with this? 58% exposure rate? That’s not negligence-that’s criminal. Someone needs to sue a district. And why aren’t there gluten-free cafeterias? It’s 2025. This isn’t rocket science.
Heidi Thomas
December 14, 2025 AT 21:04stop overcomplicating it. no gluten. period. if your kid eats a crumb and gets sick, you’re the problem. not the school. not the food industry. you. fix your kitchen.
Alex Piddington
December 16, 2025 AT 13:46the fact that bone age delay is a predictor of catch-up potential is profound. it means the body is still resilient. even if growth has stalled, the window isn’t closed. that’s hope encoded in radiology.
Jordan Wall
December 18, 2025 AT 12:33larazotide acetate? sounds like snake oil to me. if diet is the only proven treatment, why are we wasting millions on ‘shields’? the real solution is education. teach parents how to read labels. fix the supply chain. stop chasing pharma magic bullets.
Shofner Lehto
December 20, 2025 AT 08:06every parent should know: if your child is small, tired, or anemic, test for celiac before you assume it’s ‘just how they are.’ it’s not laziness. it’s not pickiness. it’s a silent autoimmune storm. early detection saves lives.
Benjamin Sedler
December 20, 2025 AT 16:16gluten-free yogurt? sure. but did you check the malt flavoring? it’s barley. it’s gluten. it’s hidden. and yeah, I’ve seen a kid get hospitalized after a ‘safe’ yogurt. one ingredient. one mistake. one lifetime of consequences.
michael booth
December 20, 2025 AT 18:45the statistical outcomes are unequivocal: 98% of children diagnosed before age five reach full adult height with strict dietary adherence. this is not a borderline medical condition. it is a medical imperative. we must prioritize screening in pediatric wellness visits.
Gillian Watson
December 20, 2025 AT 19:54my cousin’s daughter was diagnosed after her brother got it. she had zero symptoms. just… didn’t grow. now she’s 14, tall, plays soccer, eats gluten-free pizza like it’s normal. it’s wild how quiet this disease can be.
Martyn Stuart
December 21, 2025 AT 10:31don’t forget: cross-contamination isn’t just in kitchens. it’s in shared fryers, in bakery cases, in restaurant grills. even if you’re perfect at home, school, parties, and restaurants are minefields. always ask. always double-check.
Chase Brittingham
December 22, 2025 AT 14:36the emotional toll on teens is real. my nephew stopped going to birthday parties because he didn’t want to be ‘the gluten kid.’ it took a counselor and a support group to get him back. this isn’t just about food-it’s about belonging.
Rudy Van den Boogaert
December 22, 2025 AT 16:01my daughter was diagnosed at 6. We switched diets, started supplements, tracked growth monthly. Within 8 months, her iron was normal. At 18 months, she was on the 50th percentile. No magic. Just consistency. And yes, it’s expensive. But worth every penny.
Pavan Kankala
December 23, 2025 AT 12:15gluten-free is a corporate scam. Big Pharma and Big Food are pushing this so they can sell overpriced bread. Your kid just needs more protein. And maybe less school stress. This whole thing is overdiagnosed.