Warfarin Interactions: What You Need to Know About Drug and Food Risks
When you're taking warfarin, a blood thinner used to prevent dangerous clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. Also known as Coumadin, it's one of the most commonly prescribed anticoagulants—but it's also one of the trickiest to manage because even small changes in your diet or other meds can throw off your dose. Warfarin doesn't work the same for everyone. Your body’s response depends on genetics, liver function, and what else you're taking or eating. A single change—like drinking a glass of green tea or starting a new antibiotic—can send your INR (the test that measures how long it takes your blood to clot) too high or too low. Too high, and you risk bleeding. Too low, and you risk a stroke or clot.
One of the biggest factors affecting warfarin is vitamin K, a nutrient that helps your blood clot naturally, directly opposing warfarin’s effect.Vitamin K1 is found in leafy greens like spinach, kale, broccoli, and Brussels sprouts. You don’t need to avoid these foods—just keep your intake consistent. If you normally eat a salad every day, keep doing it. If you rarely eat greens, don’t suddenly start eating a pound of kale a week. Sudden shifts confuse your body and make your INR unstable. Another major concern is herbal supplements, many of which interact with warfarin in unpredictable ways.St. John’s wort, for example, can speed up how fast your body breaks down warfarin, making it less effective. Garlic, ginkgo biloba, and ginger can increase bleeding risk. Even green tea, often seen as harmless, can interfere when consumed in large amounts. And then there are the medications, including common ones like antibiotics, pain relievers, and even some heart drugs.Amoxicillin, for instance, can boost warfarin’s effect. Ibuprofen and naproxen can raise bleeding risk when taken with warfarin. Even some antifungals and seizure meds can change how warfarin works.
It’s not just about what you take—it’s about what you stop taking. Many people don’t realize that quitting a medication cold turkey can be just as risky as starting one. If your doctor tells you to stop an antibiotic or switch painkillers, always check how it affects your warfarin. Your INR should be checked more often during these changes. And if you’re ever unsure—call your pharmacist. They see these interactions every day.
Below are real stories and practical guides from people who’ve navigated these risks. You’ll find advice on how to talk to your doctor about interactions, what herbal teas to avoid, and how to spot warning signs when warfarin isn’t working right. This isn’t theoretical. These are the mistakes people make—and how to avoid them.
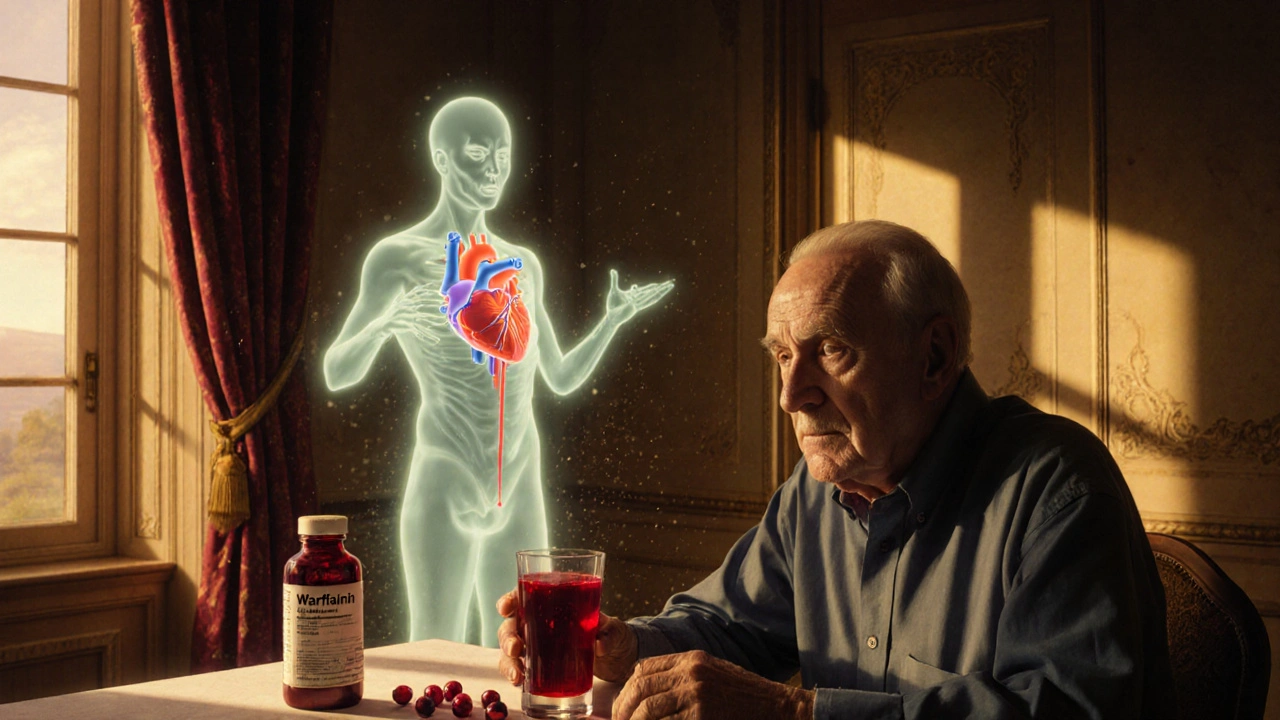
Cranberry products can dangerously increase warfarin's effects, raising INR levels and risking life-threatening bleeding. Learn why even small amounts pose a threat and what safer alternatives exist.
Read More