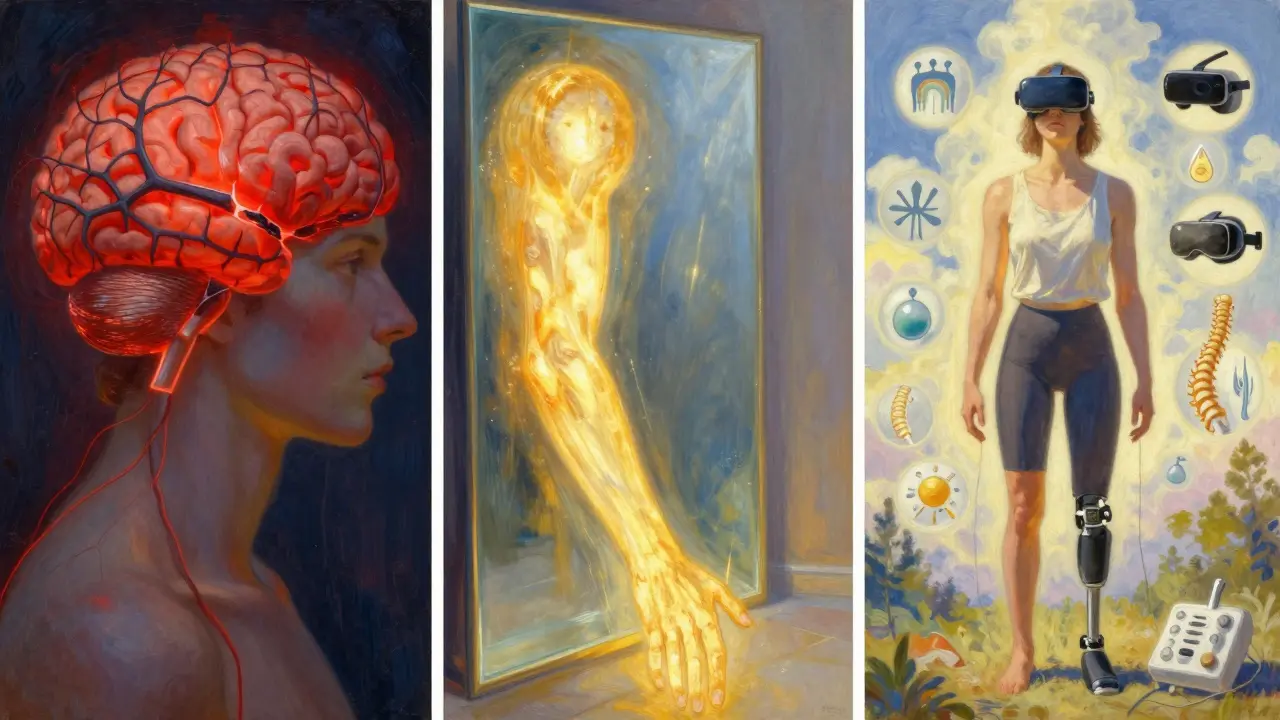
When someone loses a limb, their body doesn’t just lose a part-it loses a sense of that part too. But for many, the limb doesn’t disappear from their mind. Instead, it hurts. This is phantom limb pain (PLP), and it’s not in your head. It’s in your brain. And your spinal cord. And your nerves. It’s real, measurable, and affects 60% to 85% of amputees. If you or someone you know is dealing with this, you’re not alone-and you don’t have to just live with it.
Think about it: you feel a sharp cramp in your missing foot, or a burning sensation in your hand that’s no longer there. It’s not a memory. It’s not imagination. Brain scans show the exact same areas lighting up as if the limb were still attached. That’s because your nervous system didn’t just shut down-it rewired. And that rewiring can cause chaos.
What Phantom Limb Pain Really Feels Like
People describe phantom limb pain in ways that sound impossible: tingling like pins and needles, crushing pressure, electric shocks, or deep aching cramps. The pain usually shows up in the farthest parts of the missing limb-like fingers or toes-even if the amputation was higher up. It often starts within days or weeks after surgery, but sometimes doesn’t show up for months.
It’s not the same as stump pain. Stump pain is at the cut end of the limb-maybe from scar tissue, nerve damage, or an ill-fitting prosthesis. Phantom pain is deeper, stranger. It feels like the limb is still there, twisted, clenched, or burning. And it can get worse with stress, cold weather, fatigue, or even a bad night’s sleep.
Some people get it for a few weeks and it fades. But if it’s still there after six months? The chances of it going away on its own are almost zero. That’s not a myth. That’s what the clinical reviews say.
Why Your Brain Keeps Sending Pain Signals
Your brain maps your body. Every finger, toe, knee, and shoulder has a little spot in your sensory cortex. When you lose a limb, that spot doesn’t vanish. It gets quiet. But other parts of your brain-like those for your face or upper arm-start to take over. It’s like a neighborhood where one house burns down, and the neighbors move into the empty lot. They start using it, even if it wasn’t meant for them.
When you touch your cheek, the signal doesn’t just go to your face anymore. It spills over into the area that used to belong to your missing hand. Your brain gets confused. It thinks, “Wait-that’s my hand being touched.” And if that area is already wired to send pain signals? You feel pain in your phantom hand.
This isn’t just theory. MRI and PET scans prove it. When someone with PLP reports pain, the brain region that once controlled their lost limb lights up. That’s why treatments that target the brain-like mirror therapy-can actually work.
Medications: What Works and What Doesn’t
Most people start with meds. And for good reason: they’re fast, widely available, and often covered by insurance. But not all pills work the same for everyone.
- Tricyclic antidepressants like amitriptyline and nortriptyline are the most common first-line treatment. They’re not for depression here-they help calm overactive nerves. Doses start low (10 mg at bedtime) and slowly go up. Many report 40-50% pain reduction, but side effects like drowsiness, dry mouth, and weight gain make some quit.
- Anticonvulsants like gabapentin and pregabalin were originally for seizures, but they calm nerve pain too. Gabapentin often starts at 300 mg a day and can go up to 3,600 mg. About 72% of users on Reddit said it helped, but 58% stopped because of dizziness or brain fog.
- NSAIDs like ibuprofen and naproxen? They help a little at first, especially if there’s inflammation around the stump. But for true phantom pain? Only 65% get relief, and most lose that benefit after a few months.
- NMDA blockers like ketamine (given IV) are for tough cases. They block a brain chemical linked to chronic pain. Results can be dramatic-but they’re not for home use. Side effects include dizziness, hallucinations, and high cost.
- Opioids like oxycodone or morphine? They’re used, but controversial. The American Pain Society warns against using more than 50 morphine milligram equivalents (MME) daily. Long-term use leads to dependence in about 35% of users. They’re a last resort, not a solution.
- Botox injections might sound odd for pain, but they work for some. When injected near neuromas (tangled nerves at the stump), they can reduce pain by 60-70% for up to 12 weeks. It’s not a cure, but it’s a break.
The bottom line? Most people need to try two or three meds before finding one that works. And even then, it’s rarely 100%. That’s why many turn to non-drug options.

Mirror Therapy: Seeing Is Believing
Mirror therapy is simple. You sit in front of a mirror, place your intact limb on one side, and your stump on the other, hidden behind the mirror. You move the good limb slowly while watching its reflection. To your brain, it looks like you’re moving the missing limb.
This tricks your brain. The visual feedback says, “Your hand is moving. It’s not in pain.” Over time, that rewires the confusion. The brain stops sending pain signals because it’s getting a new message: the limb is okay.
It’s not magic. It takes daily practice. 15 to 30 minutes a day, for weeks. Some people quit after two weeks because they don’t see results fast. But studies show that those who stick with it for 6-8 weeks often cut their pain by half.
One 2023 case study followed a man who had 8/10 pain for 18 months. After 45 days of mirror therapy, his pain dropped to 3/10. He didn’t need more meds. He didn’t need surgery. Just a mirror and consistency.
There are mirror boxes you can buy. Or you can make one with a cardboard box and a piece of glass. The key isn’t the tool-it’s the repetition.
Other Non-Medication Options
If meds and mirrors aren’t enough, there are more tools:
- TENS (Transcutaneous Electrical Nerve Stimulation): A small device sends mild electric pulses through pads on your stump. It blocks pain signals. Studies show 30-50% of users get relief. It’s safe, cheap, and FDA-cleared.
- Spinal cord stimulation: A tiny device is implanted near your spine. It sends pulses that interrupt pain signals before they reach the brain. In recent trials, 65% of patients saw major pain reduction. It’s surgery, but for those with severe, unrelenting pain, it’s life-changing.
- Biofeedback: You learn to control your body’s responses-heart rate, muscle tension-using monitors. It doesn’t erase pain, but it helps you manage the stress that makes it worse.
- Virtual reality (VR): The next step beyond mirrors. Instead of a reflection, you see a digital limb moving in sync with your good limb. Early trials show promise, especially for people who struggled with mirrors. By 2027, experts predict VR will boost adherence to over 80%.
None of these are magic bullets. But together? They shift the game. The most successful patients don’t just take pills. They combine treatments.
What Experts Say About Long-Term Management
Doctors don’t treat PLP like a broken bone. You don’t fix it and move on. It’s a chronic condition that needs ongoing care. The best outcomes come from teams: a pain specialist, a physical therapist, a neurologist, and sometimes a psychologist.
One big myth? That good pain control during surgery stops PLP. Research now shows it doesn’t. Even with epidurals and strong pain meds during amputation, PLP still develops in most cases. That’s why early intervention after surgery matters more than ever.
And it’s not just about pain levels. It’s about quality of life. People with uncontrolled PLP are more likely to get depressed, avoid prosthetics, or isolate themselves. Treating the pain isn’t optional-it’s essential for recovery.
Real People, Real Results
One woman in Birmingham, who lost her leg after a car accident in 2022, tried three antidepressants before finding one that helped. She still had sharp pain. So she started mirror therapy. At first, she felt silly. But after six weeks, she could put on her prosthesis without flinching. She now uses it daily.
A man on Reddit shared he tried gabapentin, then TENS, then Botox. Nothing worked alone. But when he added mirror therapy? His pain dropped from 9/10 to 4/10. He calls it “the glue that held everything together.”
On the flip side, a man who relied only on opioids for three years ended up dependent. He had to go to rehab. His pain didn’t go away. He’s now on a combination of pregabalin, mirror therapy, and monthly TENS sessions. He says, “I’m not cured. But I’m living again.”
What You Should Do Next
If you’re dealing with phantom limb pain:
- Don’t wait. If it’s been over six months, don’t assume it’ll fade. Seek help.
- Start with low-dose amitriptyline or gabapentin. Talk to your doctor about side effects.
- Get a mirror box. Try mirror therapy for 20 minutes a day, every day, for at least six weeks.
- Consider TENS. It’s affordable, non-invasive, and safe to try at home.
- Join a support group. The Amputee Coalition has over 12,000 members. Talking to someone who’s been there changes everything.
- Keep track. Rate your pain daily. Note what helps and what doesn’t. That info is gold for your doctor.
There’s no single cure. But there’s a path. And it’s not just about drugs. It’s about your brain. Your body. And your persistence.
Is phantom limb pain real, or is it just in my head?
It’s real. Brain scans show clear activity in areas that once controlled the missing limb during pain episodes. It’s not psychological-it’s neurological. The pain comes from nerve rewiring in your spinal cord and brain, not from emotions or imagination.
How long does phantom limb pain last?
For some, it fades in weeks. But if it lasts more than six months, it’s unlikely to go away without treatment. Studies show persistent PLP after this point has a slim-to-none chance of resolving on its own. Early intervention is key.
Can mirror therapy really help, or is it just a fad?
Yes, it’s backed by science. Mirror therapy works by tricking the brain into seeing movement in the missing limb, which helps correct faulty nerve signals. Studies show 50-70% of users get meaningful pain reduction after 6-8 weeks of daily use. It’s not a cure, but it’s one of the most effective non-drug treatments available.
Why do some medications stop working over time?
Your body can build tolerance to drugs like gabapentin or antidepressants, especially with long-term use. Also, phantom pain involves multiple brain pathways. A drug that works on one pathway may not touch others. That’s why combining treatments-like meds plus mirror therapy-is often more effective than relying on one.
Are opioids safe for treating phantom limb pain?
Opioids can help in severe cases, but they’re risky. The American Pain Society recommends limiting use to under 50 morphine milligram equivalents (MME) per day due to addiction risks. About 35% of long-term users develop dependence. They’re not a long-term solution-only a last resort when other treatments fail.
What’s the newest treatment for phantom limb pain?
In January 2024, the FDA approved a new spinal cord stimulation device called Evoke by Saluda Medical. It adjusts stimulation in real time based on your pain signals, and in trials, it reduced pain by 65% on average. Also, virtual reality versions of mirror therapy are entering trials and may boost adherence by over 80% by 2027.

Haley DeWitt
February 15, 2026 AT 16:04John Haberstroh
February 17, 2026 AT 00:01Carrie Schluckbier
February 18, 2026 AT 14:35guy greenfeld
February 18, 2026 AT 14:46Adam Short
February 18, 2026 AT 23:00Sam Pearlman
February 20, 2026 AT 06:47Steph Carr
February 20, 2026 AT 20:12Liam Earney
February 21, 2026 AT 11:03Oliver Calvert
February 22, 2026 AT 22:48Prateek Nalwaya
February 24, 2026 AT 02:03