Herbal Tea & Medication Interaction Checker
Enter your prescription medication to see if it has known interactions with common herbal teas. Remember: This tool is not a substitute for professional medical advice.
Potential Interactions
Note: Only 17% of known herb-drug interactions have been proven in human studies. This tool shows potential risks based on current medical knowledge. Always consult your healthcare provider.
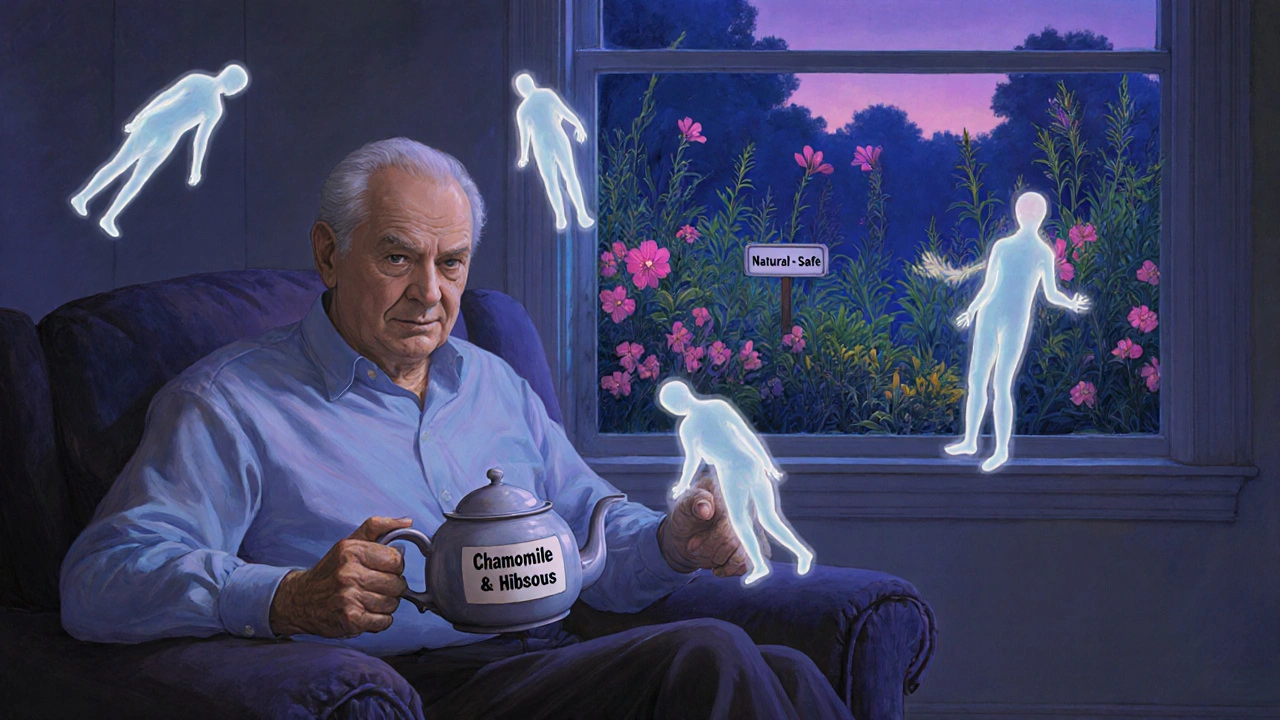
Many people drink herbal teas thinking they’re harmless-just a warm, natural sip of comfort. But if you’re taking prescription medications, that cup of chamomile, hibiscus, or green tea could be doing more than soothing you. It might be changing how your drugs work-sometimes dangerously.
Why Herbal Teas Aren’t Just ‘Herbal’
Herbal teas aren’t tea in the traditional sense. They don’t come from the Camellia sinensis plant. Instead, they’re made from roots, flowers, leaves, or seeds of other plants-chamomile, peppermint, echinacea, hibiscus, St. John’s wort, and more. People drink them for sleep, digestion, immunity, or just because they taste good. But unlike pharmaceuticals, these teas aren’t tested for safety before they hit store shelves. The FDA treats them as food, not medicine. That means no proof of effectiveness, no required warning labels, and no standard dosing.That’s a problem when you’re on medications that need to stay in a very narrow range to work. Drugs like warfarin, digoxin, cyclosporine, and theophylline have tiny windows between helping you and harming you. Even small changes in how your body absorbs or breaks them down can lead to serious side effects.
Green Tea: The Silent Drug Thief
Green tea is one of the most common herbal teas-and one of the most dangerous when mixed with certain drugs. It’s not just about caffeine. The real issue is epigallocatechin gallate (EGCG), a powerful antioxidant that interferes with how your body moves drugs around.A 2023 study showed that drinking three cups of strong green tea daily cut the blood levels of nadolol, a beta-blocker used for high blood pressure and heart rhythm issues, by 85%. That’s not a small drop. It means the drug isn’t working. Your heart rate might spike, your blood pressure could climb, and you might not even realize why.
Green tea also messes with statins. Atorvastatin, a cholesterol-lowering drug, saw its effectiveness drop by 31-39% in people who drank green tea regularly. That’s a big deal if you’re trying to avoid a heart attack or stroke. The reason? Green tea blocks transporters in your gut and liver-OATP1A1 and OATP1A2-that are needed to get these drugs into your bloodstream. It’s like putting a lock on the door your medicine needs to walk through.
St. John’s Wort: The Fast-Track to Drug Failure
St. John’s wort is often used for mild depression. But if you’re on antidepressants, birth control, blood thinners, or even some cancer drugs, this tea can make them useless.It turns on an enzyme in your liver called CYP3A4. This enzyme breaks down drugs faster than normal. So instead of staying in your system long enough to work, your medication gets flushed out too quickly. Studies show it can drop levels of cyclosporine (used after organ transplants) by up to 50%. That could lead to organ rejection. It can also make birth control fail, leading to unplanned pregnancies.
The National Center for Complementary and Integrative Health says St. John’s wort interacts with more than 50 different medications. And most people have no idea. They think, “It’s natural, so it’s safe.” But natural doesn’t mean harmless.
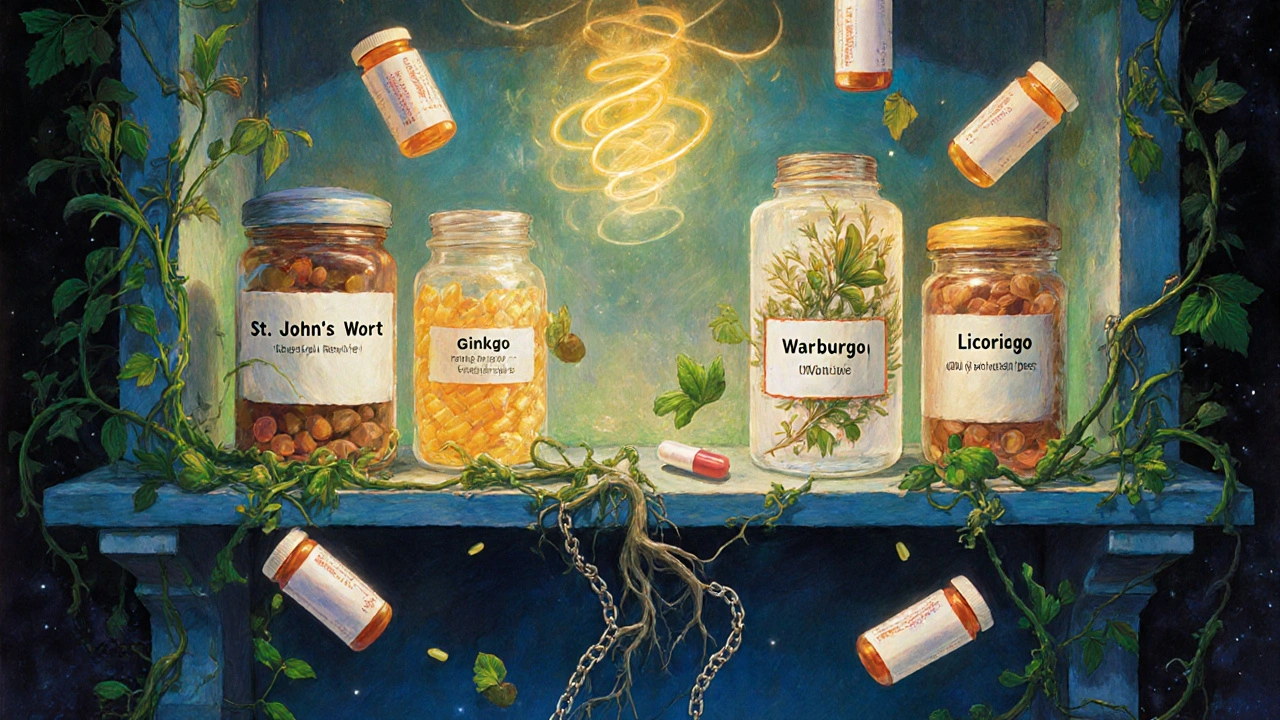
Chamomile, Hibiscus, and Ginkgo: The Bleeding Risks
Chamomile tea sounds gentle. But it contains apigenin, a compound that may interfere with how your body processes hormones. Early research suggests it could reduce the effectiveness of oral contraceptives by affecting liver enzymes.Hibiscus tea is popular for lowering blood pressure. Sounds good, right? But if you’re already taking lisinopril or another ACE inhibitor, hibiscus can push your blood pressure too low. There are documented cases where patients dropped below 90 mmHg systolic-leading to dizziness, fainting, and even falls.
Ginkgo biloba tea (or supplements) is often taken for memory. But it thins the blood. When combined with warfarin, aspirin, or even ibuprofen, it can increase your risk of bleeding-sometimes severely. The American Heart Association warns people on blood thinners to avoid ginkgo, garlic, and ginseng. And yet, many still drink it thinking it’s “just a tea.”
Goldenseal and Licorice: Hidden Triggers
Goldenseal, sometimes brewed as a tea for colds, blocks two major liver enzymes: CYP2D6 and CYP3A4. That means it can either make drugs build up to toxic levels or stop them from working at all. Over 50% of prescription drugs are affected by these enzymes. That includes antidepressants, painkillers, heart meds, and even some antibiotics.Licorice root tea is used for sore throats and digestion. But it can lower potassium levels. If you’re on diuretics (water pills) or heart medications like digoxin, that’s a recipe for dangerous heart rhythms. The FDA has flagged licorice as a risk for people with high blood pressure or heart conditions.
What You Should Do Right Now
If you’re taking any prescription medication and drink herbal teas regularly, here’s what to do:- Make a list. Write down every tea, supplement, or herbal remedy you take-name, how often, how much. Don’t forget the ones you only drink once a week.
- Bring it to your doctor. Don’t wait for them to ask. Many doctors assume herbal teas are safe and won’t bring it up. But you need to tell them. A 2022 Mayo Clinic review found only 25% of older adults disclose herbal use to their providers.
- Be specific about brewing. A weak cup of chamomile is different from a strong, steeped pot. Concentration matters. Tell your doctor how strong your tea usually is.
- Avoid concentrated extracts. Capsules, tinctures, and powders are far more potent than brewed tea. Stick to brewed teas if you must use them, and even then, be cautious.
- Watch for changes. If you start a new tea and notice new dizziness, fatigue, bruising, irregular heartbeat, or changes in mood or sleep, stop the tea and call your doctor.
Who’s at Highest Risk?
You’re more vulnerable if you:- Take medications with a narrow therapeutic index (warfarin, digoxin, cyclosporine, theophylline, lithium)
- Are over 65 and on multiple medications (polypharmacy)
- Have liver or kidney disease
- Take antidepressants, blood thinners, or heart medications
- Use herbal teas daily, not just occasionally
The FDA and NCCIH both warn that older adults are the most at-risk group. They’re the ones most likely to be on multiple meds and most likely to drink herbal teas for “natural” relief. But they’re also the least likely to tell their doctors about it.
The Bigger Picture
The herbal tea market is booming. It’s expected to hit over $11 billion by 2027. Companies market blends for “immunity,” “detox,” “stress relief,” and “energy.” But there’s no oversight. No labeling requirements. No warnings about drug interactions.Even the word “tea” tricks people. They don’t think of it as a supplement. But it’s still a bioactive substance. A cup of green tea isn’t just a drink-it’s a chemical compound interacting with your body’s systems.
Research is still catching up. Only 17% of known herb-drug interactions have been proven in human studies. That means we might be missing half the risks. Until we know more, caution is the only safe strategy.
Bottom Line
Herbal teas aren’t inherently bad. But they’re not harmless, either. If you’re on medication, treat them like you would any other drug: with respect, awareness, and open communication with your healthcare provider. Don’t assume “natural” means safe. Don’t wait for a problem to happen before you ask. Talk to your doctor. Bring your tea list. Your health depends on it.Can I still drink herbal tea if I’m on blood thinners?
It depends on the tea. Avoid ginkgo, chamomile, ginger, garlic, and hibiscus teas-they can increase bleeding risk. Green tea is also risky because it may interfere with how your body processes the medication. Stick to plain peppermint or rooibos, but still tell your doctor what you’re drinking. Never stop or change your blood thinner without medical advice.
Does green tea affect statins?
Yes. Drinking strong green tea daily can reduce the effectiveness of atorvastatin by up to 39%. It blocks the transporters your body needs to absorb the drug. If you’re on a statin, it’s safest to avoid green tea altogether-or at least limit it to one weak cup per day and monitor your cholesterol levels closely with your doctor.
Is chamomile tea safe with birth control?
There’s evidence chamomile may reduce the effectiveness of oral contraceptives by interfering with liver enzymes that break down hormones. While human studies are limited, the risk is real enough that it’s not worth taking. If you rely on birth control, avoid chamomile tea or use a backup method. Talk to your OB-GYN.
Can I drink hibiscus tea if I have high blood pressure?
If you’re already taking blood pressure medication like lisinopril, hibiscus tea can lower your pressure too much-sometimes dangerously. There are documented cases of systolic pressure dropping below 90 mmHg. If you want to use hibiscus for blood pressure, do it under medical supervision, not as a replacement for your prescribed treatment.
What should I tell my doctor about my herbal teas?
Tell them the exact name of the tea, how often you drink it, how strong it is (e.g., steeped for 5 minutes or 10), and whether you use loose leaves, bags, or concentrates. Don’t say “I drink herbal tea sometimes.” Be specific. Many doctors don’t realize teas can interact with meds-so your details could prevent a serious problem.
Don’t let a warm cup of tea become a silent health risk. Your body is a complex system. What you put in it matters-especially when you’re already managing medication. Stay informed. Speak up. Your next cup of tea shouldn’t be a gamble.

Daisy L
November 21, 2025 AT 22:46So let me get this straight-my chamomile tea is basically a silent assassin for my birth control?? And I thought my ex was the problem!! 😱 I’ve been drinking this stuff since college like it’s water-now I’m sweating bullets thinking I’ve been one steep away from a baby I didn’t plan!!
Sammy Williams
November 22, 2025 AT 20:55Yikes. I drink green tea every morning with my statin. Guess I’m switching to peppermint now. My cardiologist never mentioned this. Thanks for the heads-up-this could’ve been bad.
Julia Strothers
November 23, 2025 AT 13:53Of course the FDA treats herbs like candy. They’re in bed with Big Pharma. Why would they warn you? If you knew your chamomile tea could save you from a $500 pill, the whole system collapses. They don’t want you to know. They want you dependent. This is control. This is chemical enslavement. And they call it ‘natural’ to make you feel safe while they poison you slowly. Wake up.
Erika Sta. Maria
November 25, 2025 AT 00:18Actually, in Ayurveda, we’ve known for 5000 years that herbs interact with medicines-what’s new? You westerners just discovered this because you love pills more than plants. Also, ginkgo? That’s just a fancy name for a brain tonic. You think your brain needs a patent to work? LOL. Also, typo: it’s ‘St. John’s wort’ not ‘St. Johns wort’-you’re welcome.
Nikhil Purohit
November 26, 2025 AT 13:21Really glad someone laid this out clearly. I’m on warfarin and I drink hibiscus tea every night for my blood pressure. I had no idea. Going to stop it tomorrow and talk to my doc. Thanks for the warning-this is the kind of info that saves lives.
Debanjan Banerjee
November 26, 2025 AT 14:34Let’s be precise: EGCG in green tea inhibits OATP1A2 transporters, reducing systemic absorption of statins and beta-blockers. The 39% reduction in atorvastatin levels is backed by a 2023 RCT in the Journal of Clinical Pharmacology. Also, St. John’s wort induces CYP3A4 and P-glycoprotein-this isn’t folklore, it’s pharmacokinetics. If you’re on immunosuppressants or anticoagulants, this isn’t a ‘maybe,’ it’s a hard stop. Please, stop treating herbs like tea and start treating them like drugs. Because they are.
Steve Harris
November 27, 2025 AT 20:17I appreciate how thorough this is. I’ve been drinking licorice root tea for my digestion and didn’t realize it could mess with my digoxin. I’m going to stop it and talk to my pharmacist. I think the biggest issue is that we assume ‘natural’ = safe, but that’s just not true. Thanks for the reminder to be careful and talk to our doctors.
Michael Marrale
November 29, 2025 AT 14:35Wait… so if I drink green tea, am I basically helping Big Pharma by making my meds less effective? And then they sell me more pills? That’s genius. They’re not selling health-they’re selling dependency. And the FDA? They’re just the front desk. This is a trap. Someone’s making billions off this. I’m not drinking tea anymore. Ever.
David vaughan
December 1, 2025 AT 05:16Wow. I’ve been drinking chamomile tea every night for years… and I’m on lisinopril. 😳 I just… I didn’t think. I’m so glad I read this. I’m going to stop it tonight. And tell my doctor. Thank you. 🙏
David Cusack
December 2, 2025 AT 20:19One must question the epistemological framework under which herbalism is classified as ‘food’ rather than ‘pharmacological agent.’ The FDA’s regulatory lacuna reflects a broader cultural infantilization of the consumer. One wonders whether this is negligence-or complicity. The tea-drinker, in their naivety, becomes a willing participant in their own pharmacological exploitation. The irony is not lost on those who have read Foucault.
Elaina Cronin
December 4, 2025 AT 01:50I cannot believe how many people are unaware of these interactions. I work in a pharmacy, and I’ve seen patients end up in the ER because they thought ‘herbal’ meant ‘safe.’ It breaks my heart. Please, if you take any medication-no matter how common-tell your pharmacist and your doctor about every tea, supplement, or tincture you consume. Even if you think it’s ‘just a little.’ It’s not just about you-it’s about your family, your caregivers, your future.
Willie Doherty
December 5, 2025 AT 18:24There is a significant gap between public perception and clinical evidence regarding herbal-drug interactions. The data is sparse, yes-but the mechanisms are well-documented. Until regulatory bodies mandate labeling and clinician education, the burden falls on the patient. This article is not alarmist. It is necessary. The fact that only 25% of older adults disclose herbal use is a systemic failure. We need mandatory disclosure protocols in EHRs. Not optional. Mandatory.