Bronchospasm Type Identifier
Select the symptoms and triggers you're experiencing to identify the likely type of bronchospasm.
Identified Type:
Asthmatic: Caused by chronic airway inflammation in people with asthma, often worsened by allergens, cold air, or stress.
COPD-related: Occurs in chronic obstructive pulmonary disease when the already narrowed airways tighten further, typically after infections or exposure to irritants.
Exercise-induced: Temporary narrowing of the airways during or after intense physical activity, especially in cold, dry environments.
Medication-induced: Reaction to certain drugs such as β-blockers, non-selective NSAIDs, or contrast agents used in imaging.
Anaphylactic: Part of a severe allergic reaction where airway muscles contract alongside swelling and hives.
When your airways suddenly tighten and breathing becomes a struggle, you’re likely experiencing a bronchospasm. Understanding why it happens-and that there isn’t just one kind-can make the difference between a quick fix and a serious health crisis.
What is Bronchospasm?
Bronchospasm is a sudden constriction of the bronchial muscles that narrows the air passages, reducing airflow and causing wheezing, coughing, and shortness of breath. The spike in smooth‑muscle tone can be triggered by inflammation, allergens, or even certain medications. While the term sounds clinical, most people first notice it during an asthma flare‑up or an allergic reaction.
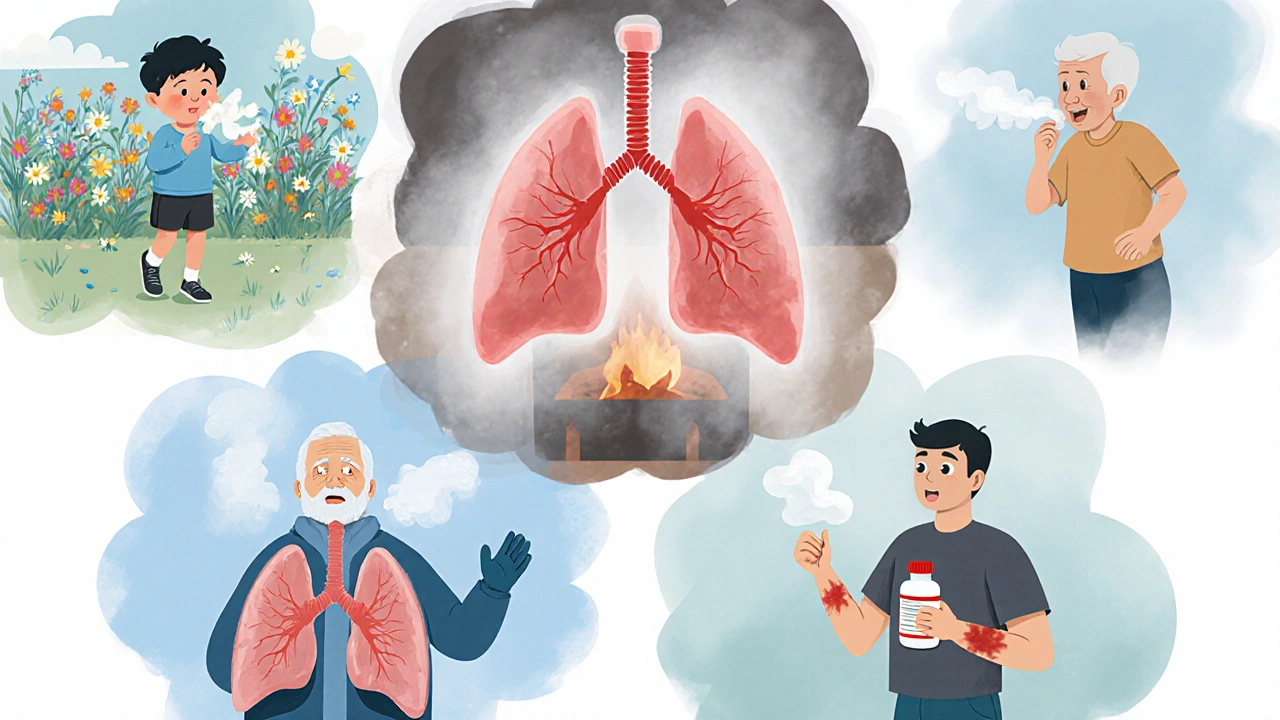
Why Not All Bronchospasms Are the Same
Think of bronchospasm as a roadblock. Different causes build the barrier in different ways, and each roadblock needs a slightly different way around it. Below are the most common types, each with its own typical trigger and management strategy.
Major Types of Bronchospasm
- Asthmatic bronchospasm caused by chronic airway inflammation in people with asthma, often worsened by allergens, cold air, or stress.
- COPD‑related bronchospasm occurs in chronic obstructive pulmonary disease when the already narrowed airways tighten further, typically after infections or exposure to irritants.
- Exercise‑induced bronchospasm (EIB) a temporary narrowing of the airways during or after intense physical activity, especially in cold, dry environments.
- Medication‑induced bronchospasm a reaction to certain drugs such as β‑blockers, non‑selective NSAIDs, or contrast agents used in imaging.
- Anaphylactic bronchospasm part of a severe allergic reaction where airway muscles contract alongside swelling and hives.
How Each Type Differs in Presentation
While wheezing and shortness of breath are common threads, the timing and accompanying symptoms can clue you into the specific type.
| Type | Common Triggers | Key Symptoms | Typical Onset |
|---|---|---|---|
| Asthmatic | Allergens, cold air, viral infection, stress | Wheeze, cough, chest tightness | Minutes to hours |
| COPD‑related | Respiratory infections, smoke, pollutants | Dyspnea, productive cough | Hours to days |
| Exercise‑induced | Running, swimming, cold‑dry air | Wheezing, throat tightness after activity | 5‑15 minutes post‑exercise |
| Medication‑induced | β‑blockers, aspirin, radiographic contrast | Sudden dyspnea, possible rash | Immediately to few minutes |
| Anaphylactic | Food allergens, insect stings, latex | Wheezing, swelling, hypotension | Seconds to minutes |
Diagnosing the Exact Type
Because treatment hinges on the cause, clinicians use a blend of history, physical exam, and targeted tests.
- Detailed symptom diary: noting when symptoms appear, activity level, and exposures helps pinpoint triggers.
- Spirometry: measures forced expiratory volume (FEV1). A reversible drop after a bronchodilator suggests asthma‑related bronchospasm.
- Peak flow monitoring: especially useful for exercise‑induced cases; athletes often record values before and after training.
- Allergy testing: skin prick or serum IgE tests identify allergic contributors to anaphylactic bronchospasm.
- Medication review: a clinician cross‑checks current prescriptions for known bronchospasm‑triggering agents.
When the cause remains unclear, a trial of inhaled bronchodilators can both relieve symptoms and serve as a diagnostic clue-rapid improvement points to a reversible airway component.
Managing Each Type Effectively
One-size‑fits‑all doesn’t work. Below are evidence‑based strategies tailored to each bronchospasm variant.
- Asthmatic bronchospasm: daily inhaled corticosteroids to control inflammation, short‑acting β₂‑agonists (SABA) for rescue, and avoiding known allergens.
- COPD‑related bronchospasm: long‑acting bronchodilators (LABA or LAMA), pulmonary rehabilitation, and prompt antibiotics for exacerbations.
- Exercise‑induced bronchospasm: use a SABA 15 minutes before activity, warm‑up routines, and consider a daily low‑dose inhaled steroid if attacks are frequent.
- Medication‑induced bronchospasm: discontinue the offending drug, substitute with a safer alternative, and treat acute symptoms with nebulized bronchodilators.
- Anaphylactic bronchospasm: immediate intramuscular epinephrine, followed by airway support, antihistamines, and corticosteroids.
In all cases, having a written action plan-complete with when to use rescue inhalers and when to call emergency services-reduces panic and improves outcomes.
Prevention Tips You Can Start Today
Even if you’ve never had a severe episode, these habits lower the odds of any bronchospasm.
- Keep an up‑to‑date allergy profile list of known triggers and sensitivities and avoid exposure whenever possible.
- Maintain optimal indoor air quality: use HEPA filters, control humidity, and keep mold at bay.
- Stay vaccinated against influenza and pneumococcus-respiratory infections are a leading catalyst for COPD and asthmatic bronchospasms.
- Review all prescribed meds annually with your doctor; ask specifically about bronchospasm risk.
- For athletes, incorporate a proper warm‑up and consider using a pre‑exercise inhaler if previously diagnosed with EIB.
When to Seek Emergency Care
Bronchospasm can escalate quickly, especially in anaphylaxis. Call emergency services if you notice any of the following:
- Rapidly worsening shortness of breath that doesn’t improve with a rescue inhaler.
- Chest tightness accompanied by a feeling of ‘air hunger’.
- Swelling of the lips, tongue, or face (signs of anaphylaxis).
- Blue‑tinged lips or fingertips, indicating low oxygen.
- Loss of consciousness or severe dizziness.
Time is critical; prompt epinephrine or advanced airway support can be lifesaving.
Frequently Asked Questions
Can bronchospasm happen without an underlying disease like asthma?
Yes. Short, isolated episodes can occur after intense exercise, exposure to cold air, or as a reaction to certain drugs, even in people with no chronic lung disease.
Why do some people wheeze more at night?
Nighttime bronchi tend to be more reactive due to cooler temperatures and reduced cortisol levels. Allergens in bedding can also trigger late‑night bronchospasm, especially in asthma.
Are inhalers the only treatment option?
Inhalers are frontline, but systemic steroids, leukotriene modifiers, and biologic agents (e.g., omalizumab) are used for severe or refractory cases. For medication‑induced bronchospasm, stopping the offending drug is key.
Can children outgrow bronchospasm?
Many children with mild asthma see reduced episodes as they age, but the underlying airway hyper‑reactivity can persist. Regular monitoring is still recommended.
Is there a test that predicts exercise‑induced bronchospasm?
A standardized exercise challenge test, where spirometry is performed before and after a 6‑minute run, reliably identifies EIB. A drop in FEV1 of ≥10% post‑exercise confirms the diagnosis.

Julia Gonchar
October 4, 2025 AT 16:16So, to break it down, there are basically five major bronchospasm categories: asthmatic, COPD‑related, exercise‑induced, medication‑induced, and anaphylactic. Each has its own typical triggers-think allergens or cold air for asthma, infections for COPD, intense workouts for EIB, certain drugs for medication‑induced, and severe allergens for anaphylaxis. The symptoms overlap a lot-wheezing, shortness of breath, chest tightness-but the timing can give clues; asthma and EIB hit within minutes, COPD may build over hours, anaphylaxis can strike in seconds. Treatment follows the cause: inhaled steroids and rescue inhalers for asthma, bronchodilators plus antibiotics for COPD flare‑ups, pre‑exercise inhalers for EIB, stopping the offending drug for medication‑induced, and immediate epinephrine for anaphylaxis. Keeping a symptom diary and knowing your triggers is the best first step.
Annie Crumbaugh
October 5, 2025 AT 17:16Totally, just jotting down when it happens helps a lot.
Vic Harry
October 6, 2025 AT 18:16Bronchospasm is just a tight lung get meds fast
Suman Wagle
October 7, 2025 AT 19:16Oh, sure, because a simple “tight lung” description totally captures the cascade of inflammatory mediators, neural reflexes, and potential life‑threatening hypoxia that can follow. But hey, if you know the basics-avoid triggers, have a rescue inhaler, and call 911 when it doesn’t quit-you're already ahead of the game.
Neil Sheppeck
October 8, 2025 AT 20:16Hey folks, just wanted to add that the whole “one size fits all” mindset really doesn’t work when you’re dealing with bronchospasm. Think of your lungs like a choir-each section (asthma, COPD, exercise, meds, anaphylaxis) sings a different tune, and you need the right conductor to keep everything in harmony. So, whether you’re a weekend runner or someone who’s been on steroids for years, tailoring your action plan to the specific trigger can make all the difference. And don’t forget to update your plan with your doc every few months; the airway landscape can change faster than you think.
Stephanie S
October 9, 2025 AT 21:16Indeed, a well‑crafted action plan, replete with clear instructions, scheduled medication reviews, and emergency contacts, can dramatically reduce anxiety, improve adherence, and-most importantly-prevent catastrophic outcomes, especially in high‑risk scenarios such as anaphylaxis or severe COPD exacerbations.
Bradley Fenton
October 10, 2025 AT 22:16If you’re not sure which trigger is at play, try a short‑term diary of activities, meds, and environment, then share it with your pulmonologist.
Wayne Corlis
October 11, 2025 AT 23:16Isn't it just wonderful how the medical literature loves to give us a tidy list of bronchospasm types, as if the human body were a well‑organized spreadsheet?
First, we have asthmatic bronchospasm, which apparently shows up whenever someone dares to inhale a pollen grain or run outside on a chilly morning.
Then there's the COPD‑related variant, because why should smokers have any mercy left when a cold sneezes at them?
Exercise‑induced bronchospasm gets a special mention, as if sprinting on a treadmill truly deserves a diagnosis separate from plain old breathlessness.
Medication‑induced bronchospasm is just the universe's way of reminding us that the pills meant to help us can sometimes betray us in the most theatrical fashion.
And of course, anaphylactic bronchospasm, the dramatic climax of an allergic reaction that turns your airway into a constricted tunnel of doom.
Each type comes with its own 'common triggers', a phrase that suggests a neat categorization while reality throws a messy cocktail of allergens, stress, and sheer bad luck at you.
The symptoms-wheeze, cough, chest tightness-are essentially the body's polite way of saying, 'Hey, I'm having a hard time keeping the air flowing, could you fix it?'
But the timing, dear reader, is where the fun begins: minutes for asthma, hours for COPD, seconds for anaphylaxis, and whatever the universe decides for medication reactions.
Treatment strategies are laid out like bullet points, yet the actual execution involves remembering to carry an inhaler, keeping epinephrine on hand, and tolerating the occasional side effect of steroids.
Don't forget the 'action plan', that glorious document that looks impressive on paper but often gathers dust in a drawer.
Meanwhile, researchers continue to fine‑tune spirometry thresholds, hoping to catch a subtle drop in FEV1 before the patient even notices a cough.
Patients, on the other hand, are left to navigate a labyrinth of advice, all while trying not to panic when their lips turn bluish.
So, in summary, bronchospasm is not a single villain but a mischievous crew of characters, each demanding its own script and starring role.
Understanding them requires more than just reading a Wikipedia article; it needs experience, good communication with healthcare providers, and perhaps a dash of humility.
And if you ever find yourself gasping for air, remember: the best response is not to overthink the classification, but to act quickly, use your rescue medication, and call for help if needed.
Kartikeya Prasad
October 13, 2025 AT 00:16Wow, such a poetic ode to airway constriction 🌬️😂. If I ever needed a bedtime story about bronchi, this would be it. But seriously, the take‑home? Keep that inhaler handy and maybe skip the marathon on a frosty morning. 🙈
HARI PRASATH PRASATH
October 14, 2025 AT 01:16According to my extensive literaure review, the pathophysiology of bronchospasm is far more intricate than the layman's simplifed explanations, which often neglect the nuanced interplay of cholinergic and adrenergic pathways, as well as the oft‑overlooked role of neurogenic inflammation.
Andrew Miller
October 15, 2025 AT 02:16Honestly, reading that feels like a lecture I never signed up for.
Brent Herr
October 16, 2025 AT 03:16People need to stop treating bronchospasm like a casual inconvenience and start recognizing it as a serious health threat that demands responsibility, education, and respect for medical advice.
Julius Adebowale
October 17, 2025 AT 04:16Data shows delayed treatment increases mortality rates significantly.
KISHORE KANKIPATI
October 18, 2025 AT 05:16Let’s celebrate the diversity of lung experiences-some of us battle asthma, others COPD, but we’re all united by the quest for clearer breaths and supportive communities.
Jefferson Vine
October 19, 2025 AT 06:16What if the pharmaceutical giants are quietly pushing inhalers that only address symptoms while they keep the market flooded with chronic bronchospasm cases? The truth is out there, hidden behind glossy brochures and persuasive ads, and it’s up to us to demand transparency.
Ben Wyatt
October 20, 2025 AT 07:16Remember, staying proactive with your peak flow checks and keeping an updated action plan can empower you to manage bronchospasm confidently and avoid emergency scares.